Psoriatic arthritis treatment is mainly aimed at 1) reducing joint pain and stiffness complaints and 2) inhibiting the disease activity and the associated joint damage.
Page Contents
What is Psoriatic Arthritis?
Psoriatic arthritis is a form of inflammatory rheumatism in which you also have the skin disease psoriasis. Most of the time, psoriatic arthritis starts with psoriasis.
The exact cause of psoriatic arthritis is unknown.
It is, however, certain that T lymphocytes are involved. T lymphocytes are certain white blood cells that play an important role in the immune system. They detect everything in your body that is foreign and destroy it.
For example, they ensure that you do not get sick from bacteria and viruses. In psoriatic arthritis, the T lymphocytes also attack cells that “belong”‘. You then speak of an autoimmune disease.
In an autoimmune disorder, your immune system ‘runs wild’, as it were, causing your immune system to think that good body cells are evil invaders.
Your immune system subsequently wants to expel these intruders. It releases certain substances which cause inflammation in your joints, tendons, muscles, or organs. Your immune system turns against your own body, as it were.
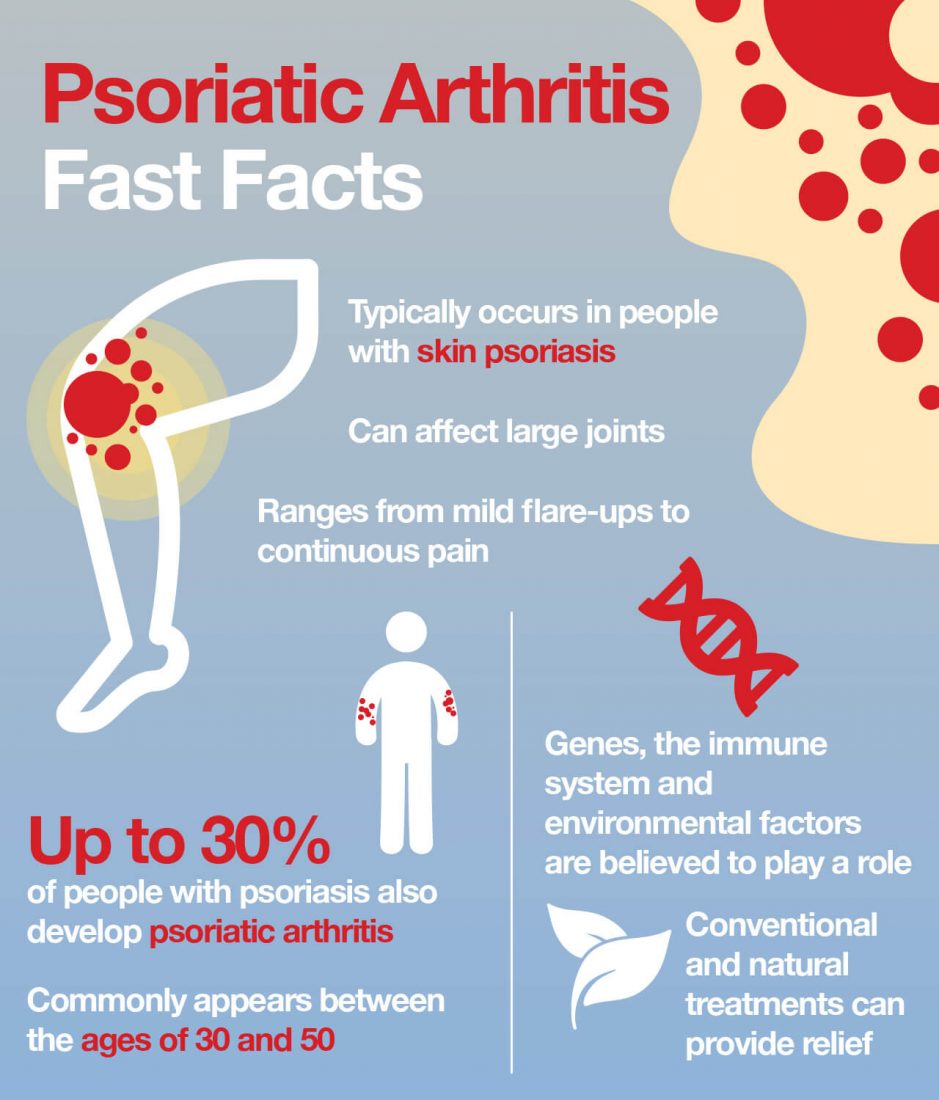
Psoriatic arthritis is more common in certain families (hereditary). If you have psoriatic arthritis, your children may get it too, but they don’t have to. There are also people with a genetic predisposition to psoriatic arthritis who do not get the condition.
Other factors that can play a role in psoriatic arthritis are stress and infections that weaken the immune system.
In addition, alcohol, smoking, and certain medicines can also play a role.
Cold and damp weather causes more complaints in many patients. Psoriatic arthritis is as common in men as it is in women. There is no correlation between psoriasis activity and arthritis activity.
Oftentimes, psoriatic arthritis starts between the ages of 30 and 50, but it can basically start at any age.
The severity of the disease varies from person to person.
Clinical Features of Psoriatic Arthritis
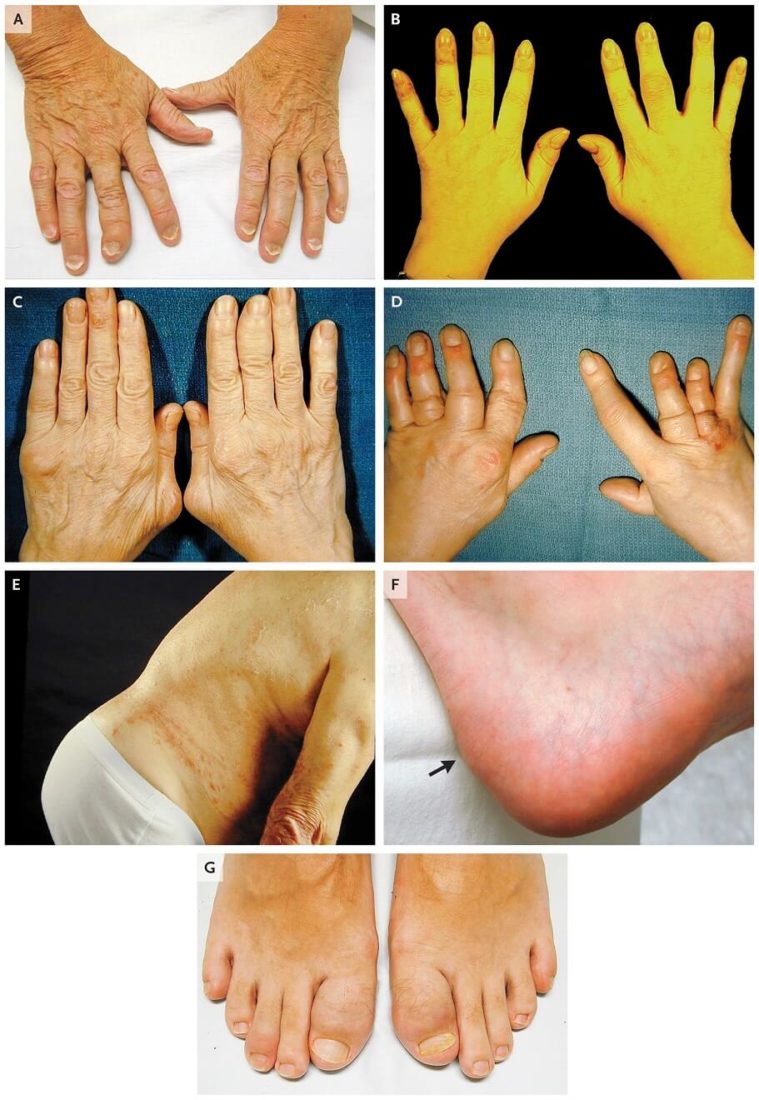
Panel A shows the distal subtype of psoriatic arthritis, with adjacent onycholysis. Panel B shows the oligoarticular
subtype. Panel C shows the polyarticular subtype. Panel D show arthritis mutilans, with telescoping of digits and
asymmetric and differential involvement of adjacent digits. Panel E shows the spondylitis subtype. Panel F shows
enthesitis of the Achilles’ tendon (arrow). Panel G shows dactylitis of the big toes. Image Source
What are the first signs of psoriatic arthritis?
In addition to the skin complaints associated with psoriasis, you also suffer from joint inflammation with psoriatic arthritis.
What happens is the lining of the joint capsule (synovial membrane) becomes inflamed. This synovial membrane and the synovial fluid provide the mobility of the joints.
The inflamed synovial membrane swells and more and more ‘inflammatory cells’ enter the fluid. Over time, the other tissues in the joints (such as cartilage and bone) also become inflamed.
Pain and stiffness are a direct result.
The inflammation and thickening of the synovial membrane affect bone, cartilage, tendons, and ligaments. This causes a lot of damage to the joint locally.
Inadequately treated psoriatic arthritis can lead to permanent disability due to fusion of the joints. Once it has occurred, the damage is irreversible.
Psoriatic Arthritis Symptoms
The most common psoriatic arthritis symptoms are:
- With psoriatic arthritis, you usually have inflammation in the body’s joints which causes stiff and painful joints in the fingers, toes, ankles, lower back, or knees.
- Sometimes inflammation in your fingers or toes occurs in the form of swelling. Your fingers and toes then look like a ‘sausage’, which is why these are called ‘sausage fingers’ or ‘sausage toes’. The medical term for this is dactylitis.

- Inflammation also occurs in the tendon attachments, for example in the Achilles tendon.
- Joint inflammation with pain, swelling, and stiffness
- Skin complaints with red spots, scaling, and itching
- Fatigue – Often there are several factors that cause and maintain the fatigue associated with psoriatic arthritis. For example, fatigue can be a direct consequence of the disease, but also a side effect of the medicines you are taking. Pain can also keep you awake at night, making you tired during the day.
- Eye inflammation due to the eyes being too dry (uveitis)
- Inflammation in the spine (in about 20 to 30% of people with psoriatic arthritis)
- Inflammation of the small vertebrae between the sternum and ribs (similar to Bechterew, spondyloarthritis)
- Inflammation of the SI joints (between the sacrum and ilium, sacroiliitis)
- Itching, allergies, and tightness (due to an excess of histamine in the blood)
With joint inflammation, the joint:
- hurts
- is swollen
- is stiff
- feels warm
- you can move less well
How is psoriatic arthritis diagnosed?
Your doctor usually bases the diagnosis on your symptoms, a physical examination, and a blood test.
During the physical exam, your doctor will look for signs of inflammation in your joints and tendons. Your doctor will monitor the mobility of your pelvis, hips, and back. Your doctor will physically examine your eyes, skin, and nails.
Usually, your doctor will have your blood tested. With the blood test, your doctor wants to find out whether inflammatory values are present in your blood and whether the hereditary factor HLA-B27 is present. The presence of HLA-B27 does not say everything because this factor also occurs in people who do not suffer from this condition.
However, if your doctor finds HLA-B27 in your blood, it can help to make the diagnosis with certainty. Often the rheumatoid factor and anti-CCP antibodies are also examined in the blood test. This helps to distinguish between psoriatic arthritis and rheumatoid arthritis.
Additional research
In addition, your doctor often conducts additional research. He will have one or more X-rays taken to see if any abnormalities are visible in the joints in your arms or legs.
How Does Psoriatic Arthritis Proceed?
Usually, periods in which you have many complaints alternate with periods in which the condition calms down on its own.
There is no connection between skin complaints and joint complaints.
Medicines also help to reduce your symptoms.
Occasionally, people with psoriatic arthritis have long-term inflamed joints.
Psoriatic Arthritis Treatment
Psoriatic arthritis is a type of tissue pain.
It is important that the different types of pain, namely nerve pain, tissue pain, and mixed pain, are all treated in their own way.
Psoriatic arthritis has no cure, and treatment varies from person to person. The disease progresses differently for everyone and the complaints are often different.
Psoriatic arthritis treatment is mainly aimed at reducing joint pain complaints and inhibiting disease activity and the associated joint damage.
What is the treatment for psoriatic arthritis?
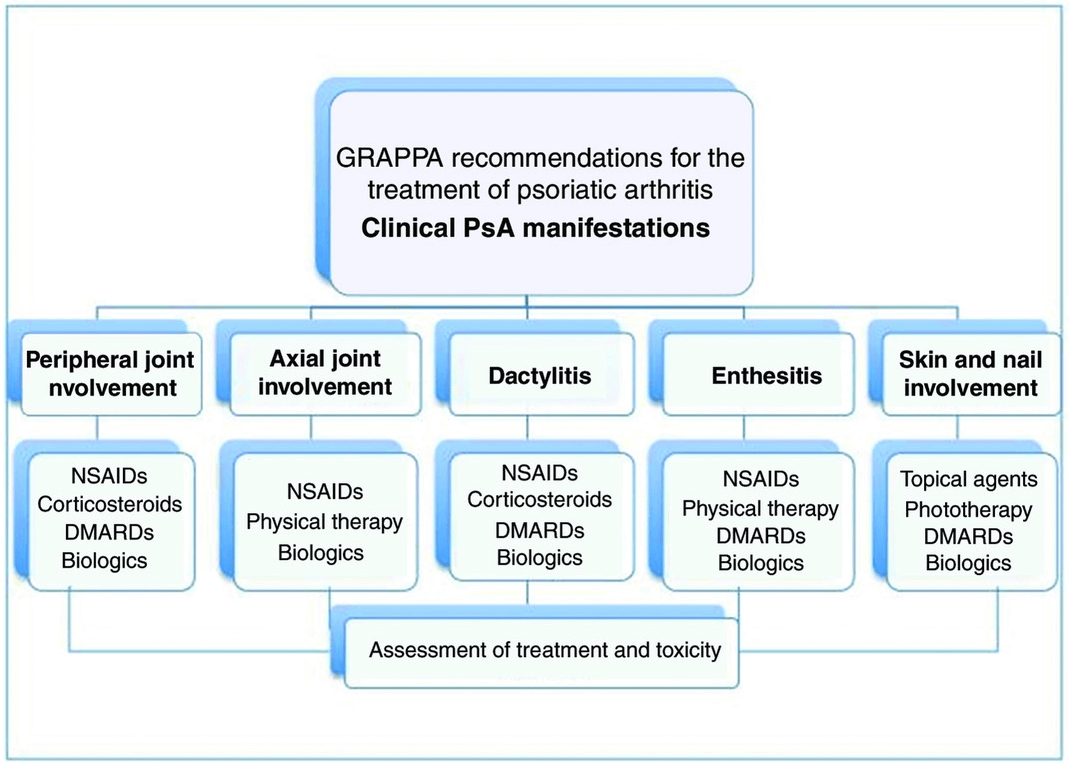
1. NSAIDs (non-steroidal anti-inflammatory drugs)
NSAIDs are often prescribed as a psoriatic arthritis treatment option. It aims to inhibit inflammation and counteract pain and stiffness. However, they can also cause stomach complaints. For this reason, an agent that protects the stomach is often prescribed in addition to NSAIDs.
In general, 2 types of anti-inflammatory drugs are used; NSAIDs and steroids.
- NSAIDs are mainly used to reduce symptoms of pain, swelling, and stiffness. Examples of NSAIDs are ibuprofen, naproxen and diclofenac.
- Corticosteroids or glucocorticoid drugs, such as cortisone, hydrocortisone, prednisone, and prednisolone, also suppress the inflammatory activity, so that there is less pain and swelling in the joints. These agents are also able to somewhat inhibit joint damage.
2. DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
Since most of the joint damage begins in the first two years of the disease, the ideal psoriatic arthritis treatment is a particularly rapid treatment at an early stage of the disease.
There are drugs that, in addition to relieving symptoms, also suppress the activity of the disease itself.
These drugs are called DMARDs (Disease-Modifying Anti-Rheumatic Drugs), such as methotrexate and sulfasalazine. DMARDs are prescribed by the medical specialist.
DMARDs can inhibit and prevent joint and cartilage damage. Many patients achieve demonstrable improvement with the help of these medications, but joint damage cannot be completely prevented with DMARDs.

3. Biological DMARDs (biologicals)
When the DMARDs prove to be ineffective, a switch can be made to treating psoriatic arthritis with biological DMARDs.
Organic DMARDs are also called biologicals. Sometimes the treatment with biologicals is combined with DMARDs. The name ‘biological’ refers to the fact that these agents can mimic the action of the body’s own proteins.
To be eligible for biological DMARDs, the patient must meet certain criteria. Your rheumatologist and dermatologist can inform you about the requirements.
TNF-alpha inhibitors are mainly used in patients with PsA. It has been found that these patients have a greatly increased amount of TNF-alpha in their bodies. As a result, inflammation in the joints is constantly stirred up. Too much TNF-alpha in PsA also causes irregularities in the skin.
An advantage of treatment with biologicals is that not only the symptoms in joints are addressed but also on the skin and nails.
4. TNF-alpha (Tumor Necrosis Factor)
TNF-alpha (Tumor Necrosis Factor) is an inflammation-stimulating substance, which is naturally present in the body. The main task of this substance in psoriatic arthritis treatment is to initiate and maintain inflammation.
TNF-alpha belongs to the group of messenger substances (cytokines); substances through which inflammatory cells communicate with each other. The substances attach themselves to specific recipient cells of the immune system to transmit their message and thus play an important role in the inflammatory process.
Biologicals, such as TNF inhibitors, ensure that these cytokines cannot attach to these so-called receptors (receivers) so that the message to inflame does not get across. In this way, inflammation is inhibited and prevented.

Additional psoriatic arthritis treatments
It is good to keep moving, despite your joint problems. This prevents your muscles and joints from further weakening and losing stability.
A physiotherapist or remedial therapist can help you to keep moving and to deal with your pain complaints. For example, he gives advice on which exercises you can do to keep your joints flexible and strengthen your muscles. He also guides you in finding a balance between exercise and rest.
In addition to exercise, it is important to eat a healthy and varied diet, with lots of fruit and vegetables. There is no special diet that has been shown to work for psoriatic arthritis.
Try to maintain a healthy weight. With a healthy weight, you have less risk of joint problems and cardiovascular disease.
What can you do about psoriatic arthritis?
It is important that you are regularly monitored by your attending medical specialist.
Not only will he/she monitor your medication and keep an eye on the course of your illness, but the specialist can also answer your questions and give you advice as and when needed.
The rheumatologist will mainly deal with your joint complaints and the dermatologist with skin problems.
If you use biologicals, it is important that your treating doctors consult each other about this. Sometimes the tasks of the specialists are taken over by a consultant or a specialist nurse. This person can also provide you with important information, especially in a practical area.
Living with PsA
It’s quite something to be told you have a chronic illness.
After all, no cure has yet been found for this chronic disease and often puts a heavy burden on the quality of life. PsA doesn’t just affect your life; your partner, your children, your family, and your friends and colleagues will also have to learn to live with your illness.
Sometimes things go much better for periods and then worsens for a while.
It is often difficult to explain to those around you why you can one day do something and not the next. Yet that is exactly where the solution lies. Try to explain it, make sure people understand your situation. Maybe explaining is a bit tiring at first, but you will benefit greatly from this in the long run.
Exercise is very beneficial when you suffer from arthritis. This helps keep the joints flexible and the muscles around the joints strong, reducing pain and stiffness. You can go to a physiotherapist for this. He can apply exercise therapy. Exercise therapy works on muscle strengthening and coordination of the muscles around certain joints.
Conclusion
It is impossible to predict how PsA will develop.
The disease can be of a mild character, but can also be just as serious as, for example, rheumatoid arthritis.
PsA is a chronic disease, which means there is no cure.
The symptoms of the disease can be alleviated and nowadays the progress of the disease can also be slowed down if one becomes aware of it in time.
People with PsA especially, experience a lot of skin problems and the disease can also cause psychological complaints. Don’t trivialize this, talk to your doctor about it and find a solution together.