In this comprehensive guide, we discuss those types of psoriasis identified by medical research and the most common symptoms associated with each of these types of psoriasis. Pictures of the different psoriasis types make identification easier.
Page Contents
What is Psoriasis?
Do you suffer from itchy, red, scaly patches? Then you may be dealing with psoriasis. This skin condition can be very annoying.
Psoriasis is a chronic skin condition that currently affects more than 125 million people globally; i.e. 2-3% of the world population. In the US, about 8 million people are affected by psoriasis.
Psoriasis is an immune-mediated inflammatory disease (IMID). In other words, it’s a disease where the cause is not clear but is identified by skin inflammation brought on by a dysfunction in the body’s immune system. The visible result of the inflammation is scales and plaques which are generally red and they itch.
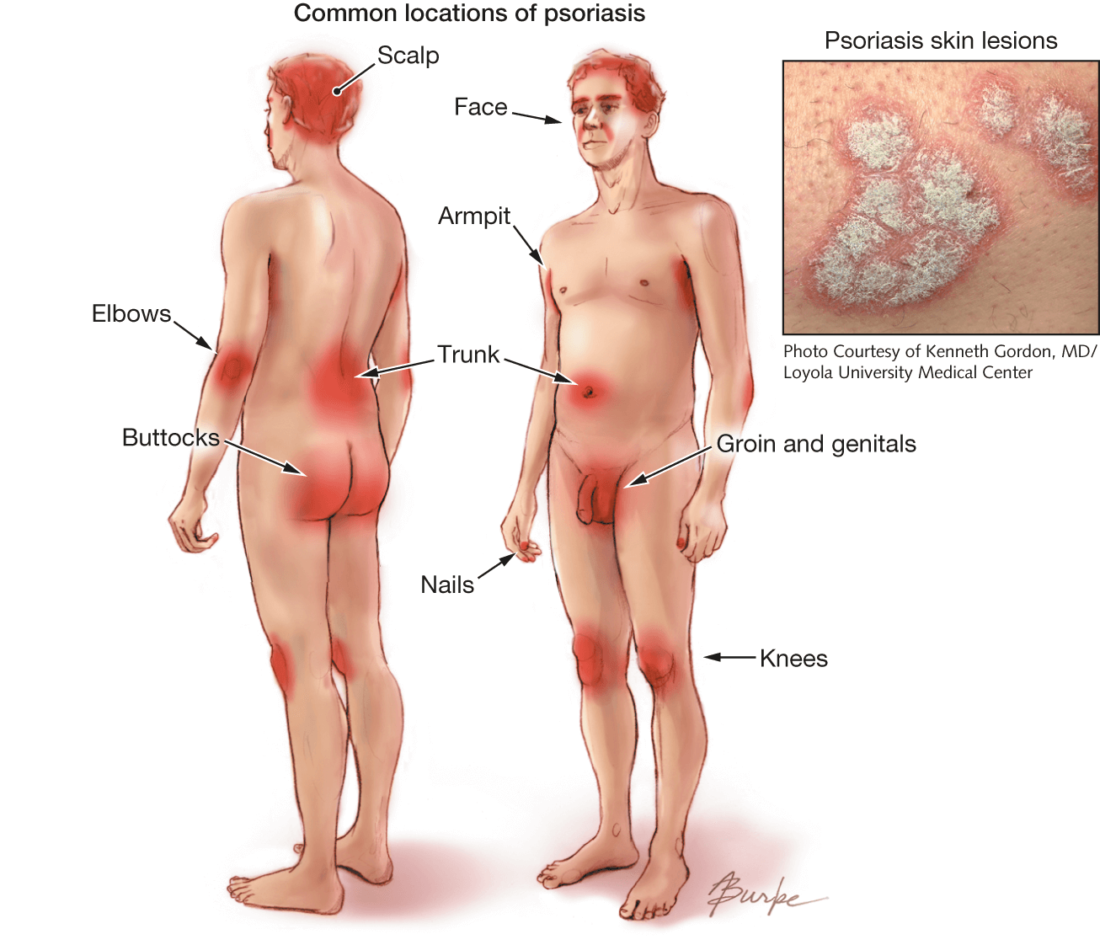
Psoriasis plaques may sting, itch, and burn. They are generally found on the scalp, elbows, face, back, palms, feet, genital area, and knees. The plaques can, however, also appear on other parts of the body. Psoriasis affects both males and females and people of all skin colors.
Inflammation brought on by psoriasis can unfortunately also impact body tissue and other organs in the human body. Other health issues are also possible. About one-third of people with psoriasis are affected by PsA (psoriatic arthritis).
What Causes Psoriasis?
An overactive immune system leads to accelerated cell growth every 3-4 days whereas, in normal skin renewal, skin cells grow and fall off in thirty days.
Your skin is made up of several layers. The top layer, the epidermis, is constantly renewed. Old skin cells die, flake off unnoticed, and new skin cells take their place.
In psoriasis, too many new skin cells are being produced. These skin cells should mature properly before replacing old ones, but they don’t.
As a result, the new skin flakes off, and inflammation occurs, because the skin is not protected well enough against invaders such as bacteria and viruses from the outside.
Unfortunately, it is not known exactly what causes the accelerated growth of skin cells.
There are clear indicators that heredity plays a role. If you have psoriasis yourself, someone else in your family often has this predisposition too. The chance that you will develop psoriasis if one of your parents has psoriasis is 10%. The chance of getting psoriasis if both parents have psoriasis is 50%.
Psoriasis Triggers
Some of the most common psoriasis triggers include but are not limited to:
- Stress
- Flu
- Throat inflammation or other infections. Common bacterial infections like strep throat and thrush can cause an outbreak. Get immediate treatment for these infections.
- Certain medications such as anti-malarial drugs (plaquenil and chloroquine), beta-blockers (high blood pressure), lithium (used to treat bipolar disorder), interferons (treatment for leukemia, cancer, hepatitis, etc.), terbinafine (synthetic antifungal available in both oral and topical formations is used to treat jock itch, athlete’s foot, etc.), and NSAIDs (ibuprofen)
- In women, hormonal changes that take place during puberty and menopause
- Damage to the skin. Do you have a scrape, cut, or burn? Psoriasis can develop one to two weeks later
- It appears that psoriasis is more common in people who smoke and drink alcohol. “Alcohol opens the blood vessels in the skin. When your blood vessels are dilated, white blood cells, including the T cells that are believed to be responsible for psoriasis, can sneak into the outer layers of your skin more easily — and you don’t need to be inviting more T cells.” Source
- Foods such as white potatoes, peppers, tomatoes, eggplant, dairy products, pork, red meat, shellfish, foods high in sugar and fats, and gluten (found in wheat, barley, and rye). Are eggs bad for psoriasis? Yip. Eggs, dairy products, and red meat all contain a polyunsaturated fat called arachidonic acid which promotes inflammation.
- Very cold and dry weather, as well as heaters, dry out the skin. A humidifier is highly recommended during harsh weather conditions to keep the skin hydrated
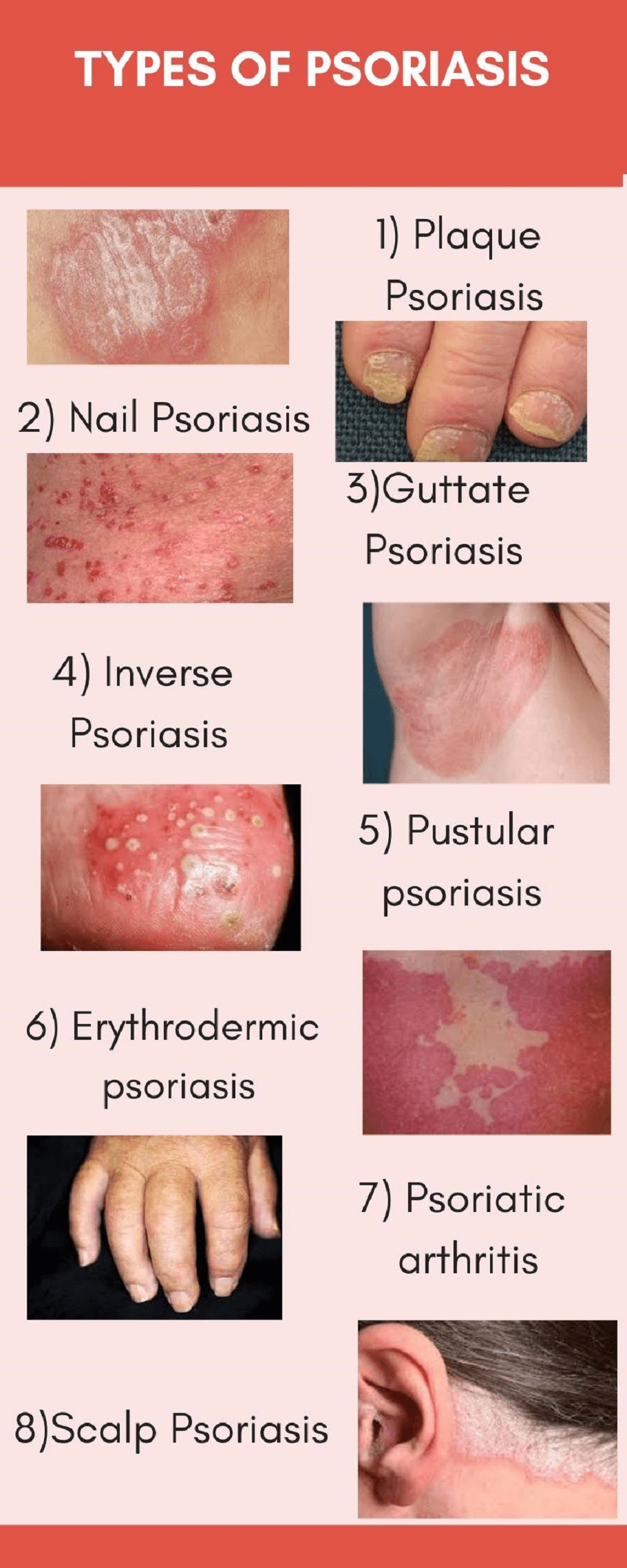
What are the different types of psoriasis?
- Plaque psoriasis (Psoriasis Vulgaris)
- Guttate psoriasis
- Inverse psoriasis (Flexural Psoriasis)
- Pustular Psoriasis (5 different kinds)
- Acropustulosis of infancy
- Palmoplantar Pustulosis (PPP or LPP – Localized Pustular Psoriasis)
- Von Zumbusch Psoriasis (Generalized Pustular Psoriasis – GPP)
- Annular Pustular Psoriasis (APP)
- Impetigo Herpetiformis (IH) (aka generalized Pustular Psoriasis of Pregnancy – PPP)
- Psoriatic Erythroderma (Exfoliative Psoriasis)
- Psoriatic Arthritis (PsA)
- Scalp Psoriasis (Psoriasis Capitis)
- Nail Psoriasis (Psoriatic Onychodystrophy or Psoriatic Nails)
- Genital psoriasis
Plaque Psoriasis (aka Psoriasis Vulgaris)
Plaque psoriasis (psoriasis Vulgaris or chronic plaque psoriasis) is the most common form of psoriasis. About 80% of people with psoriasis have psoriasis Vulgaris.
This form is characterized by red spots on the skin with white flakes on top. The spots can be itchy and usually occur on the arms, legs, back, or buttocks.
The plaques are covered with thick, silvery, shiny scales. They appear gradually or with the appearance of triggers.

Symptoms of psoriasis Vulgaris:
- Red spots with white or silver-gray scaling
- Itchy patches (especially when they just appear)
- Large and/or small plaques
- Dry skin
- Single or multiple areas on the skin
- Spots mainly on the elbows, knees, back, and buttocks
- Flakes come off easily
- Can be permanent or temporary
Besides psoriasis Vulgaris, there are a number of other types of psoriasis. These types are mainly characterized by their location on the human body. Below are some other forms of psoriasis:
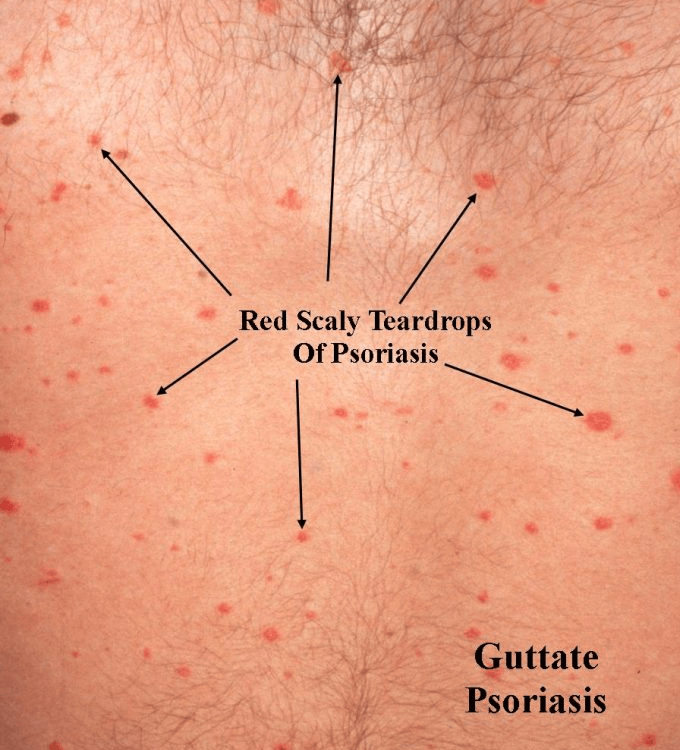
Guttate Psoriasis
Guttate psoriasis is an acute form of psoriasis in which a sudden rash develops all over the body and is characterized by reddish-pink, scaly patches the size and shape of droplets on the skin. It is sometimes referred to as “drop shape” psoriasis.
It usually develops in 10% of psoriasis patients and occurs mainly between the ages of 10 and 40. In 1 in 3 people, guttate psoriasis turns into psoriasis Vulgaris. Why this happens to some but not to others remains unknown.
Below are guttate psoriasis pictures for easy reference:

Pictures above and below courtesy https://acadderm.com/guttate-psoriasis-a-shower-of-scaly-teardrops/
What Causes Guttate Psoriasis?
Guttate psoriasis is not contagious and therefore not dangerous to other people.
Guttate psoriasis can occur in anyone, including people who have never had psoriasis before. The condition can develop very suddenly. Red spots may appear within days to weeks.
Some causes of guttate psoriasis:
- Bacterial infection. In 80% of the cases, the rash is triggered by a bacterial streptococcal infection, as a result of an inflammation of the throat or inflamed tonsils (tonsillitis). The rash then manifests itself about 2 to 4 weeks after the throat infection.
- Hereditary predisposition. People with a family history of psoriasis are known to develop some type of fever blister after being infected with the streptococcal bacteria.
- Medicines. Guttate psoriasis can develop after taking certain medications, such as NSAIDs, beta-blockers, and anti-malaria medications.
- Viral infection. Viral infections in children, such as chickenpox, rubella, and sixth disease (roseola), can lead to guttate psoriasis.
- This form is seen in people predisposed to psoriasis, with psoriasis running in families.
- For some people, guttate psoriasis is considered an initial symptom of the more common form of psoriasis (psoriasis Vulgaris).
- Guttate psoriasis can develop just like that but is more often seen after a throat infection with bacteria of the group A beta-hemolytic streptococci (Streptococcus pyogenes) or inflamed tonsils.
What are the symptoms of Guttate Psoriasis?
Guttate psoriasis can affect the whole body.
The rash often starts on the trunk, arms, or legs. After that, it can spread to the face, ears, and sometimes the scalp. Guttate psoriasis is not seen on the palms and soles.
These spots can be itchy but do not hurt. When you scratch, the flakes become even whiter. This is also referred to as the “candle wax phenomenon”. Complaints often associated with ordinary psoriasis, such as nail disorders and joint problems, are not found in psoriasis guttate.
How To Treat Guttate Psoriasis
Inverse Psoriasis (aka Flexural or Intertriginous Psoriasis)
This is a form of psoriasis that is found in the folds of the body.
Hereditary predisposition plays a major role in the development of the condition.
Major complaints are salmon-colored or pink-red plaques, which can be very itchy.
No flaky plaques are visible.
Treatment mainly focuses on symptom control.

Picture courtesy https://www.aafp.org/afp/2013/0501/p626.html

Inverse psoriasis groin pictures courtesy https://www.sciencesource.com/
What is inverse psoriasis?
Inverse psoriasis is common in people with other forms of psoriasis.
In the most common forms of psoriasis, the symptoms are mainly visible on the outside of the limbs (e.g. elbows and knees). In contrast, inverse psoriasis is mainly characterized by patches in body folds.
It therefore mainly occurs in the armpits, under or between the breasts, in the navel, in the groin, and buttock crack. In addition, it can occur behind the ear shells and on the genitals.
Note: do not confuse this form of psoriasis with a fungal infection or a venereal disease.
What causes inverse psoriasis?
As mentioned already, inverse psoriasis mainly occurs in humans who have a hereditary predisposition to the condition. With this hereditary abnormality, skin cells thicken abnormally. At the same time, an abnormal immune response develops.
This form of psoriasis is also triggered by heat and moisture, such as is commonplace in body folds. Inverse psoriasis is generally found more in people who already have psoriasis or who are overweight.
In addition, people with inverse psoriasis are more prone to fungal and yeast infections and fungal infections.
Symptoms of inverse psoriasis
Unlike the common form of psoriasis (psoriasis Vulgaris), inverse psoriasis is not associated with thick, hard, gray, scaly plaques.
Inverse psoriasis is characterized by purplish or brown lesions on dark-skinned people and bright red lesions on light-skinned people. These lesions may feel moist when you touch them. Large areas within the body folds are normally covered with lesions and can be very itchy.
In inverse psoriasis, the patches have a shiny and smooth appearance that gets worse when skin rubs against skin and the skin remains sweaty.
In addition, painful bleeding fissures may occur in the body fold areas because the skin naturally is very sensitive in those areas.
Pustular Psoriasis
This is a serious and dangerous form of psoriasis. This acute skin condition is often accompanied by pus heads, fever, and pain.
“With pustular psoriasis, the autoimmune response is even more severe. Scientists believe that it is caused by a defect in an inflammatory protein known as interleukin. Under normal circumstances, there will be a “matched set” of interleukin molecules, one that promotes inflammation and the other that tempers inflammation.
If one of the two molecules is defective, it can leave inflammation on “high” with no way to turn it off. What results is a massive burst of inflammation that kills many of the white blood cells involved in the autoimmune assault. The dead cells combined with lymph fluid creates the white, gooey substance recognized as pus”. Source
Pustular psoriasis most commonly affects the palms and soles, but may also be found on fingers and toes.
Pustular psoriasis is not contagious and as such, you cannot get infected by someone else, nor can you infect another person should you suffer from this skin disease.
Adults are usually affected by pustular psoriasis; children hardly ever.

Pustular psoriasis is identified by different types, each of which is identified by where the outbreak of blisters on the skin occurs:
- Palmoplantar pustulosis psoriasis (PPP)
- Acropustulosis of infancy
- Generalized or Von Zumbusch pustular psoriasis
- Annular Pustular Psoriasis (APP)
- Impetigo Herpetiformis (generalized Pustular Psoriasis of Pregnancy – PPP)
Palmoplantar pustulosis (PPP)
Palmoplantar pustulosis, or palmoplantar psoriasis, is a chronic, but rather rare autoimmune disease affecting the palms of the hands and/or soles of the feet.
The person affected develops various painful and itchy sores, pustules, or blisters on the affected areas. As a result, the person is no longer able to perform certain leisure or professional activities.
There is no cure, but symptoms of the condition can be relieved with a few treatments. Flare-ups do occur in many people.

How rare is palmoplantar pustulosis?
“…palmoplantar pustulosis is not a very common condition (prevalence rate <0.1%) and individuals with PPP also tend to suffer from plaque psoriasis…” Source

What are the causes of palmoplantar pustulosis?
Palmoplantar pustulosis is a non-contagious autoimmune disease in which the immune system mistakenly attacks healthy skin cells of the hands and feet.
The exact cause is unknown, but several risk factors have been identified that contribute to the development of the condition.
Smoking is more likely to trigger the disease and also any flare-ups.
Risk factors of palmoplantar pustulosis skin condition
Common risk factors include:
- The presence of another autoimmune disease such as diabetes, arthritis, coeliac disease, or a thyroid disorder
- A family history of palmoplantar pustulosis
- A family history of psoriasis (chronic skin disease with dry skin and scaling)
- Gender: The disease affects mainly women in the sixth and seventh decade of life
- Older adults are more likely to develop this form of psoriasis
- Smoking (or used to smoke) has been found to be a cause in as much as 90% of those people diagnosed with this skin condition
What causes flare-ups of palmoplantar pustulosis?
Palmoplantar pustulosis flare-ups occur more quickly due to the following factors:
- The use of some medications, such as steroids (Prednisone). Stopping with this type of drug sooner than prescribed by a doctor can cause a flare-up
- Infections, especially streptococcal infections (a type of bacteria)
- Smoking
- Stress
Symptoms of palmoplantar pustulosis
People affected develop signs of the condition on both palms and/or soles but it differs from person to person. In most people, symptoms begin with tender and red skin on the hand palms and soles of the feet.
Fluid-filled pustules, blisters, and skin ulcers (pustules) form on the red areas and often burst open. The often painful and itchy skin lesions are filled with white or yellow pus and come and go. They dry out, causing brown, flaky, cracked, thickened, and dry skin.
When pustules appear on the feet, it makes walking complicated. Other physical activities also often pose problems for patients with palmoplantar pustulosis. Certain occupations where hands are used to fulfill a task or require a lot of walking are not advisable for those people affected by this skin condition.
Diagnosis
The typical thickened scaly red callus patches in combination with the thick gray flakes on the palms can already betray the diagnosis. But sometimes it is difficult to distinguish between chronic hand eczema and fungal infection.
The doctor examines the skin lesions. He also asks about a family history of psoriasis or palmoplantar pustulosis, as well as whether other possible risk factors are present.
Furthermore, a biopsy of the skin is required to rule out infections and disorders with a similar clinical picture.
Acropustulosis (may be referred to as acropustulosis of infancy)
A type of pustular psoriasis, acropustulosis is a rare condition of the skin characterized by itching.
The condition is generally found to affect babies and referred to by some as acropustulosis of infancy or infantile acropustulosis. The rash generally appears in the first year of the baby’s life. Young children and adults can also be affected. This often occurs when the affected person got injured or had an infection.
Pustules most commonly develop on the hands and feet but can be found on the back of the hands, on the feet, the scalp, the wrists, and ankles. Spontaneous healing occurs around the age of 3 with no long-term health complications caused by the condition.
Picture courtesy https://www.contemporarypediatrics.com/view/infants-pustular-eruption-not-scabies
Symptoms of acropustulosis
Highly itchy pustules develop on the hands and feet. The pustules start out as flat, red, small bumps. When these red bumps get filled with fluid they turn into raised bumps and the pus change to a yellowish or whitish color.
The pustules show up in clusters known as crops and are very itchy. During those first years of the baby, crops come and go. Flare-ups last between 7 and 14 days and come back every two to four weeks. As the infant gets closer to 3 years old, flare-ups are less frequent.
In adults and older children, acropustulosis mainly occurs on the toes and around the fingernails. In these situations, acropustulosis can harm the finger and toenails. In severe cases, damage to the bones can be caused by acropustulosis.
Causes of acropustulosis
The cause is unknown.
One hypothesis is that it is a nonspecific reaction of the skin in predisposed patients to a specific stimulus such as infection or infestation. Scabies used to be seen as a possible cause, but recent studies do not confirm this which means it may occur without scabies as the “trigger”.
Acropustulosis is not contagious and as such, if the child has a flare-up they can still attend school or daycare.
The itchiness can make children with infantile acropustulosis restless, sad, annoyed, and cause a decrease in appetite. Sleep is often disturbed.
The clinical picture of recurrent attacks of plantar and palmar itchy pustules differentiates this disease from the other pustular eruptions at this age.
Risk factors associated with acrospustulosis
One cannot simply eliminate vulnerability to the scabies mite even though there are no studies to support this as a definite cause of acropustulosis.
It would seem the principal risk factor is being of a very young age, as this skin disease is most prevalent in infants.
Previous flare-ups of acropustulosis. For some time, you can expect your child to have more flare-ups.
In non-infant situations, any kind of skin condition or infection may make the person more susceptible to acropustulosis.
Diagnosis
Consult your pediatrician should you notice any kind of rash on your kid’s skin.
Since acropustulosis can easily be mistaken for another condition, you should not try and diagnose yourself but rather call on your doctor.
In general, a test to diagnose the skin condition of acropustulosis is not required. A physical checkup by a competent professional should be sufficient as they usually are able to differentiate between acropustulosis and chickenpox or another skin condition.
When in doubt, a simple blood test will reveal the existence of infection or any other condition. Children old enough to have been vaccinated are very unlikely to have chickenpox.
Generalized Pustular Psoriasis aka Von Zumbusch Pustular Psoriasis
Von Zumbusch psoriasis is a rare and serious form of generalized pustular psoriasis. Pustules are depicted as white pus-filled blisters which are caused by a rapid and abnormal inflammation of the autoimmune system which subsides and reappears often.
Von Zumbusch Pustular Psoriasis is not contagious. Unlike the other 2 forms of pustular psoriasis which most commonly affect hands and feet, generalized pustular psoriasis can affect large areas of the skin.
Although Von Zumbusch is rarely found in children, it can start at any age. Adults older than 50 are largely affected by this particular type of pustular psoriasis.
When children are affected by Von Zumbusch pustular psoriasis, it usually is the first time they are exposed to psoriasis and is not as severe as in adults.

Picture of Generalized Pustular Psoriasis aka Von Zumbusch Pustular Psoriasis
Some of the triggers that are known to cause flare-ups of Von Zumbusch pustular psoriasis are:
- Skin infections such as Staphylococcus aureus and Streptococcus epidermidis
- Untimely withdrawal or cutting down of corticosteroids
- Operational procedure
- Hypocalcemia (low calcium levels in the blood)
- Medications (penicillin, terbinafine, lithium, and interferon)
- Topical medications such as coal tar or anthralin
- Stress (mental and emotional), etc.
Diagnosing Von Zumbusch (Generalized Pustular Psoriasis – GPP)
A physical examination and testing of the pus is required to confirm the skin condition is indeed generalized pustular psoriasis.
The medical practitioner may also inquire about prior incidences of psoriasis, autoimmune diseases in the family, or any exposure recently to certain medications.
Hospitalization is required in most instances.
Tests that may be performed are:
- Testing for a bacterial infection (an infection does not cause pustular psoriasis; there should therefore be no traces of a virus, fungus, or bacteria in the pus sample)
- Performing a skin biopsy which will indicate superficial pustules
- To obtain a blood count (will show the prevalence of anemia, lymphopenia, neutrophilia)
- Test liver and kidney functions for impairment
- Measure electrolytes and calcium/phosphate levels
Symptoms of Von Zumbusch
Von Zumbusch pustular psoriasis starts suddenly with large areas of the skin breaking out in painful and tender red skin. Tiny, pus-filled pustules form within hours. A lot of these tiny pustules then coalesce into bigger blisters. The affected skin can become itchy. When the affected skin is scratched, it may cause the pustules to rapture.
Within a day or 2, the pustules dry out and peel, leaving the skin with a smooth and glazed surface. The peeling away of the pustules is not only very painful, but it can also cause a rapid loss of moisture resulting in severe dehydration.
Other symptoms commonly experienced include fever, lethargy, weight loss, muscle weakness, anemia, chills, racing pulse.
Severe dehydration symptoms:
- Extreme thirst
- Dry mouth
- Headaches
- Reduced urination
- Dark-colored urine
- Fatigue
- Sleepiness
- Dizziness
- Confusion
- Muscle weakness
- Rapid heart rate
- Rapid and shallow breathing
- Fever and chills
- Leg swelling
- Unconsciousness
Dehydration, especially when as severe as described above, can cause other complications such as cerebral edema (brain swelling), shock, cardiorespiratory failure, seizures, acute kidney failure, coma, and even death.
Von Zumbusch pustular psoriasis can, over time, also lead to other complications such as hair and nail loss, secondary bacterial infection, and liver damage.
According to a 2016 review in the journal Psoriasis, no less than 65% of adults with pustular psoriasis will have had a prior diagnosis of plaque psoriasis. Recurrent flares are not uncommon.
Annular Pustular Psoriasis (APP)
Annular pustular psoriasis is also referred to as subacute generalized pustular psoriasis.
“Annular pustular psoriasis (APP) is a rare form of pustular psoriasis with a chronic recurrent course and good prognosis. A review of the medical literature reveals that a disproportionately high percentage of cases of APP occurs in children. In some cases, topical therapy can clear the condition, although, in severe or recalcitrant disease, systemic therapy may be necessary.” Source

Picture courtesy https://www.aafp.org/afp/2013/0401/p513.html
Impetigo Herpetiformis (IH) (aka generalized Pustular Psoriasis of Pregnancy – PPP)
This type of pustular psoriasis only develops in pregnant women, and usually in the 3rd trimester.
One in 5 pregnant women complains of itchy skin, especially if the woman was prone to dry skin and rashes before pregnancy.
There are skin problems that can be traced back to an autoimmune disease such as neurodermatitis. This condition often worsens during pregnancy and only gets better after delivery.
But there are also skin diseases such as psoriasis, in which the condition improves significantly during pregnancy and the symptoms then come back after the birth.
Itching in the abdominal area is particularly common. The skin stretches during pregnancy and therefore becomes irritated.
Mild, moisturizing creams or special body oils can provide relief. The red or purple stretch marks caused by stretching of the skin during pregnancy cannot always be avoided despite regular creaming.
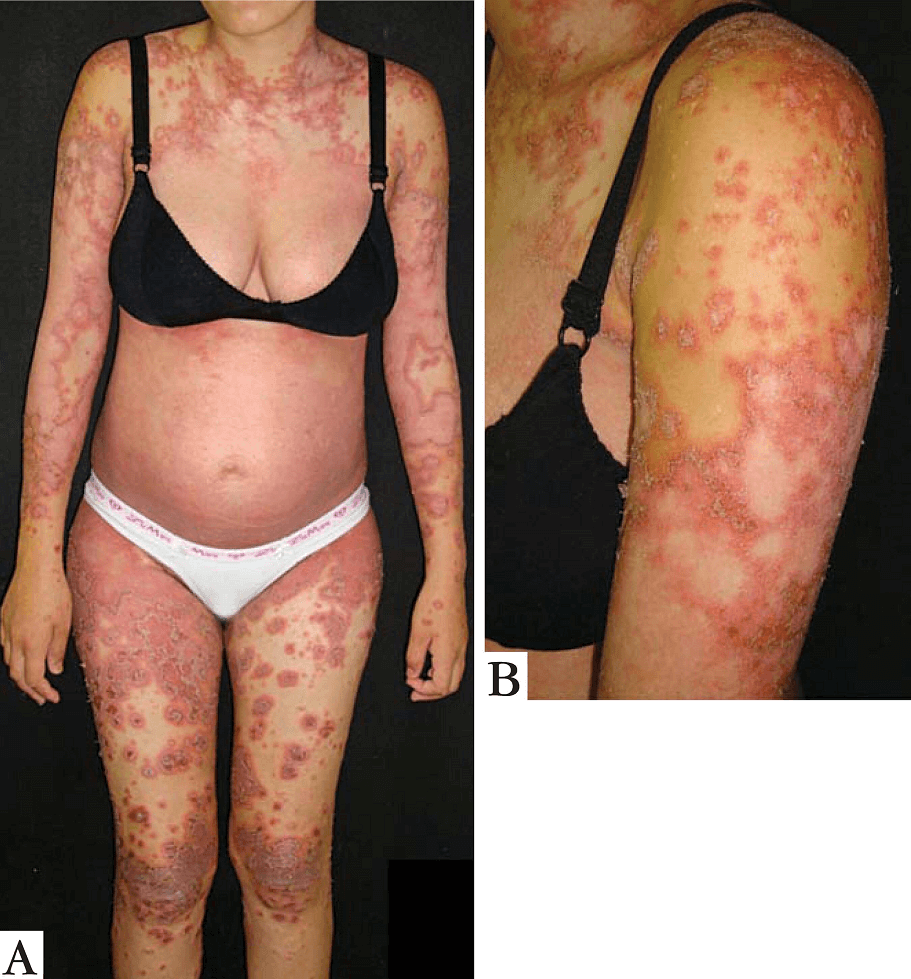
FIGURE A – 27 weeks into the first pregnancy. B- Detail of lesions on arm. Pustules on the periphery of the lesions. (Picture courtesy https://www.scielo.br/)
What Are The Symptoms Associated With Impetigo Herpitiformis?
With impetigo herpetiformis, pustules start to develop on the groin and the inner thighs.
Nausea, diarrhea, fever, chills, vomiting, and fatigue are other symptoms that present themselves in this condition. Some pregnant women indicated they experienced low calcium and phosphate levels in their blood.
As this condition poses a risk to an unborn baby, an immediate visit to the doctor is highly recommended. Some of the risks associated with impetigo herpetiformis are:
Placental insufficiency: the inability of the placenta to deliver a sufficient supply of oxygen and nutrients to the fetus. It can thus not give the baby the support it needs to develop as it should. This may subsequently lead to
- A stillbirth. The baby dies in the mother’s womb after week 20 of the pregnancy.
- Fetal abnormalities
How Is Impetigo Herpetiformis Diagnosed?
Early diagnosis is vital in order for necessary treatment to start ASAP.
It is very important to always have skin conditions assessed and clarified by a medical doctor when pregnant.
“Impetigo herpetiformis is usually diagnosed by its symptoms and its characteristic rash. A skin biopsy is typically performed to rule out other pregnancy-related conditions. Some studies have linked the condition to genetic mutations, so it is possible that some physicians may order genetic testing.” Source
There are other skin diseases apart from impetigo herpetiformis which also itch that can be seen during pregnancies.
This includes, for example, pemphigoid gestations (PG), an unpleasant autoimmune disease that only occurs in around 1 in 50,000 pregnancies.
This disease manifests itself as an itchy rash in the form of nodules and blisters around the navel, with the blisters spreading rapidly.
If it starts late in the pregnancy, it is harmless to both mother and baby.
When it starts in the first or second trimester, however, there are some complications that may occur such as premature birth or the baby is born with a similar rash.
PUPPP (pruritic urticarial papules and plaques of pregnancy) is another itchy skin condition experienced most commonly in the third trimester. The red itchy hive-like bumps appear in stretch marks on the abdomen but are not dangerous to the mother or her baby. It usually disappears after giving birth.
Erythrodermic Psoriasis (aka Psoriatic Erythroderma or Exfoliative Psoriasis)
In most cases, psoriasis is harmless. Erythrodermic psoriasis is an exception. This represents a rare but particularly aggressive and life-threatening form of psoriasis. Prompt and above all timely treatment is vitally necessary.
Those who suffer from psoriasis have basically nothing to fear. Classical psoriasis and most of its subtypes are not life-threatening. Things are different for those affected by erythrodermic psoriasis.
Only 1–3% of psoriasis patients are affected by this diagnosis. Erythrodermic psoriasis is extremely rare, making it all the more dangerous. In many cases, the disease is extremely difficult and can have life-threatening consequences for those affected.

Erythrodermic psoriasis with widespread, confluent scaly plaques courtesy https://www.aafp.org/afp/2013/0501/p626.html
Erythrodermic Psoriasis – What is it?
Erythrodermic psoriasis, often referred to as exfoliative psoriasis, is an uncommon, but extremely serious type of psoriasis. In this skin disease, more than 75% of the body of the patient has widespread, fiery, burned skin that is itchy and very painful.
This rash multiplies very quickly; subsequently requires urgent and prompt treatment by a medical specialist. Treatment can only be administered in a hospital or dermatology clinic.
“This form of psoriasis is found to mainly affect those people who already suffer from unstable plaque psoriasis. “It is often the result of an exacerbation of unstable plaque psoriasis, particularly following the abrupt withdrawal of systemic glucocorticoids.” Source
It can also happen when there is a flare-up of plaque psoriasis or Von Zumbusch pustular psoriasis.
What are the symptoms of erythrodermic psoriasis?
The symptoms may start in a gradual manner or appear suddenly.
In erythrodermic psoriasis, the widespread rash covers at least 75% of the body or in some cases, even the entire body.
The rash consists of red, scaly patches often with severe itching and pain. The fiery, red skin appears burnt. The autoimmune condition even causes peeling skin in large sheets. Pustules (tiny blisters) may also be present that is filled with pus.
The following side symptoms are common:
- Fever
- Chills
- Rapid pulse
- Joint pain
- Swollen ankles
- Muscle weakness
- Swollen lymph nodes in the groin and armpits as well
- Accelerated heartbeat.
- Hypothermia can occur since the person cannot keep him/herself warm
When should you consult a doctor?
As soon as any of these symptoms are experienced, a doctor should be consulted immediately as the disease can be life-threatening.
The doctor will question the patient about their medical history to find out if there is a history of psoriasis in the family.
He also checks for potential risk factors such as taking corticosteroids by mouth, the presence of an infection, or suddenly stopped taking psoriasis medications.
A physical exam is needed where the doctor looks for the presence of some psoriasis signs such as plaques on the skin, joint pain, and nail psoriasis.
The doctor will perform a skin biopsy, by removing some of the affected skin and having it checked in the lab for signs of psoriasis.
There is no laboratory test that can confirm that the patient has erythrodermic psoriasis, but they can rule out other causes with similar symptoms, such as atopic dermatitis, seborrheic dermatitis, and other conditions.
Triggers and risk factors of erythrodermic psoriasis
The treatment is usually successful, but occasionally a patient can no longer be helped and dies as a result of complications such as heart failure, pneumonia, or sepsis (blood poisoning).
Addressing risk factors lowers the chances of getting this aggressive type of psoriasis.
The causes of erythrodermic psoriasis are not yet fully understood. However, doctors name the following factors that are considered to likely be triggers of the disease:
- Abrupt termination of systemic psoriasis treatment
- Use of certain medications (such as anti-malarial drugs or systemic steroids)
- Infections such as HIV
- Severe sunburn
- Allergies such as an allergic reaction to some medication
- Excessive alcohol consumption
- Smoke
- Stress
- Nutrition
- Weather
- Difficult to treat psoriasis. Erythrodermic psoriasis also sometimes occurs when psoriasis (especially plaque psoriasis) is difficult to control
All of these aspects are considered risk factors and triggers for erythrodermic psoriasis. You should therefore avoid them.
Why is erythrodermic psoriasis dangerous?
Our skin plays a central role in our general health. It is the protective coat of our body and takes on vital defense and protective functions. Not only does it ward off germs, but it also regulates body temperature and protects us from losing too much fluid.
If our skin is damaged, as in the case of erythrodermic psoriasis, it loses its barrier function. As a result, the increased vulnerability of the skin can lead to life-threatening complications.
Exfoliative psoriasis often leads to a critical drop in body temperature. This in turn often leads to pneumonia or sepsis.
Other possible complications in the context of exfoliative psoriasis:
- Threateningly high loss of vital fluids,
- High mineral loss,
- Increased risk of infections,
- Kidney problems
- Heart failure
Psoriatic Arthritis (PsA)
What is Psoriatic Arthritis?
Psoriatic arthritis (PsA) is a combination of rheumatism and the skin disease psoriasis. It is a painful rheumatic disease characterized by chronic inflammation in the joints and skin-related problems.
Generally, the joints of the hands and feet, knees, wrists, and ankles are particularly affected.
This disease occurs in about 30% of people suffering from the skin disease psoriasis and, just like rheumatoid arthritis (RA), is caused by a problem in the immune system.
Psoriatic arthritis is as common in men as it is in women. There is no correlation between psoriasis activity and arthritis activity. Oftentimes, psoriatic arthritis starts between the ages of 20 and 30, but it can basically start at any age.
While people with PsA often develop psoriasis symptoms first, this is not always the case for everyone. In many people, the skin disease psoriasis does not develop until many years after the joint inflammation has started. This can complicate the diagnosis.
The intensity of the symptoms can also vary from patient to patient.
The image below: Clinical Features of Psoriatic Arthritis
“Panel A shows the distal subtype of psoriatic arthritis, with adjacent onycholysis. Panel B shows the oligoarticular subtype. Panel C shows the polyarticular subtype. Panel D show arthritis mutilans, with telescoping of digits and asymmetric and differential involvement of adjacent digits. Panel E shows the spondylitis subtype. Panel F shows enthesitis of the Achilles’ tendon (arrow). Panel G shows dactylitis of the big toes.” Source

Clinical Features of Psoriatic Arthritis
Panel A shows the distal subtype of psoriatic arthritis, with adjacent onycholysis. Panel B shows the oligoarticular
subtype. Panel C shows the polyarticular subtype. Panel D show arthritis mutilans, with telescoping of digits and
asymmetric and differential involvement of adjacent digits. Panel E shows the spondylitis subtype. Panel F shows
enthesitis of the Achilles’ tendon (arrow). Panel G shows dactylitis of the big toes. Image Source
How does psoriatic arthritis develop?
Arthritic inflammations are caused by a fault in the immune system.
In people with PsA the immune system attacks the body’s own cells; in this case mainly the joints. PsA is therefore also called an autoimmune disease.
The exact cause of this malfunction of the immune system is not yet known.
PsA is not hereditary, although it is more common in some families than others. The genetic make-up of a person can influence the development of PsA, but other factors also determine whether or not the disease is activated.
Other factors that can play a role in psoriatic arthritis are stress and infections that weakened the immune system. In addition, alcohol, smoking, and certain medicines can also play a role. Cold and damp weather causes more problems in many patients.
What happens in the joint?
In the first stage of PsA, the mucous membrane lining the joint capsule (synovial membrane) becomes inflamed. This synovial membrane and the synovial fluid provide the mobility of the joints.
The inflamed synovial membrane swells and more and more ‘inflammatory cells’ enter the fluid.
Over time, the other tissues in the joints (such as cartilage and bone) also become inflamed. Pain and stiffness are a direct result.
The inflammation and thickening of the synovial membrane affect bone, cartilage, tendons, and ligaments. This causes a lot of damage to the joint.
Inadequately treated PsA can lead to permanent disability due to fusion of the joints. Once it has occurred, the damage is irreversible.
What Does Psoriatic Arthritis (PsA) Look Like?
The symptoms of PsA can sometimes be less prevalent.
Unfortunately, it often happens that the symptoms are not recognized in time; this is partly due to the fact that abnormalities in the blood that indicate having the disease can be difficult to find.
Despite the fact that the pain in the joints is sometimes little, the damage to the joints, for example in bone erosions, can be enormous.
When you suffer from psoriatic arthritis, in addition to skin complaints as a result of psoriasis, inflammation can also occur in your joints. The inflamed area becomes warm, red, swollen and stiff, and painful.
Sitting in the same position for a long time can make the pain and stiffness worse. This makes it harder for you to move the joint.
The joints in your fingers or toes can swell painfully. You call this a sausage finger or sausage toe. The finger or toe then turns red.
Some typical symptoms of PsA are:
- Morning stiffness for several weeks
- Painful and inflamed joints (not symmetrical)
- Painful neck and back
- Excessive fatigue and lethargy
- Painful swelling of finger and toe joints
- Achilles tendon is often affected
- Eye infection due to dry eyes
- Symptoms that can occur on the skin: scaling, itching, and redness.
These symptoms can occur anywhere on the body and are by no means equally visible and intense in everyone.
Nor do they all have to occur at the same time.
Joint complaints are first noticeable in 25% of patients with PsA. However, in 75% of cases, the skin symptoms are visible first.
Changes to the nail bed and nails can also occur. PsA has also been found in 85% of patients with nail psoriasis.
How is psoriatic arthritis diagnosed?
The diagnosis of psoriatic arthritis is made on the basis of:
- History (Does the patient have psoriasis? Does it run in the family?)
- A physical examination
- A blood test
- An X-ray
PsA should mainly be distinguished from another autoimmune disease, namely, rheumatoid arthritis. Your dermatologist will refer you to a rheumatologist for the diagnosis of PsA and for setting up any treatment and guidance.
Psoriasis Capitis (Scalp Psoriasis)
Psoriasis capitis is another name for scalp psoriasis.
Important features are gray-white flakes and plaques on the hairline, which cause itching.
Hair loss does not usually occur with scalp psoriasis.
Psoriasis capitis is treated with a cream or ointment, or light therapy. There are also special shampoos.

Scalp psoriasis images above and below

What Is Psoriasis Capitis?
Psoriasis capitis is another name for scalp psoriasis. This form of psoriasis is found mainly on the hairline on the front, in the neck, and at the temples. Both men and women can suffer from psoriasis capitis. Treatment is difficult, especially for those who have a lot of hair.
Causes of scalp psoriasis
Just like normal psoriasis, psoriasis capitis is caused by an accelerated division of skin cells and an immune reaction against these skin cells. In addition, you have a higher chance of scalp psoriasis with a hereditary predisposition.
Symptoms of scalp psoriasis
Psoriasis capitis is characterized by gray-white scales. Only in people with greasy hair, these flakes will not be visible. This makes it difficult to distinguish this form of psoriasis from seborrheic eczema.
When flakes build up, plaques can form. Skin dryness can cause painful chapping and cracks. This leads to a lot of itching of the scalp. Scratching too much can cause the scalp to bleed.
Hair loss
Usually, capitis psoriasis is not associated with hair loss. Only in severe, long-lasting, and treatment-resistant forms can hair fall out in some areas. Scars can develop in these exposed areas.
Psoriasis of the nails (psoriaticonychodystrophy or psoriatic nails)
What is psoriasis of the nails?
At least half of all patients with psoriasis also have a disorder of the nails (psoriatic onychodystrophy). In 85% of people with arthritic psoriasis nail abnormalities occur. Only 5% of people with nail psoriasis have no skin or joint complaints.

Picture courtesy https://www.nejm.org
How does psoriasis of the nails develop?
It is still unclear exactly how the psoriasis of nails develops, but nail psoriasis causes problems in the area where new nails are being formed.
Nail psoriasis can develop at any age and is not contagious.
It can cause abnormalities on the nail itself, on the nail bed (area below the nail), and to the nail matrix from where nails grow. The matrix is where new cells grow and push out old cells so the nail can take on the flat and hard form characteristic of nails.
“Psoriasis of the nails is caused by the same autoimmune mechanisms as psoriasis of the skin. For reasons not entirely clear, the immune system will inexplicably regard normal tissues as harmful and launch an immune assault. Although the skin is the primary target, other tissues are affected as well. The ensuing inflammation triggers an acceleration in the production of cells, known as keratinocytes, in the skin, nails, and other tissues.
When this occurs in the skin, characteristics plaques can develop. In the fingernails and toenails, the overproduction of keratinocytes can cause thickening, malformation, and discoloration as the cells are produced faster than they can be shed.” Source
What are the symptoms of nail psoriasis?
The following abnormalities may be seen in nail psoriasis. These can be seen on the fingernails as well as on the toenails:
- Thickening and crumbling of the nail plate (aka subungual hyperkeratosis) Caused by an over-production of skin cells that accumulate between the nail plate and the nail bed. This results in the nail getting thicker, causing the nail plate to lift from the nail bed.
- The detachment of the nail plate from the nail bed starting at the tip and then proceeding towards the cuticle (aka distal onycholysis)
- Discoloration (nails become yellowish-brown)
- Holes or dents in the nail plate (aka pitting). This happens when psoriasis causes the loss of cells on the surface of the nail)
- Grooves start to form on the nail plate (aka Beau’s lines). These lines run across the nails from side to side
- White spots/lines on the nail plate (aka leukonychia). “It occurs when psoriasis induced parakeratosis affects only the intermediate and ventral matrices that form the undersurface of a nail plate. The affected area appears leukonychic (whitish) because of the internal desquamation of parakeratotic cells.” Source
How is nail psoriasis diagnosed?
The diagnosis of nail psoriasis is mainly made with the naked eye. Despite this, there are a number of other nail conditions that can look like it, including fungal nail or lichen planus (an inflammatory skin condition).
When in doubt, any of several techniques may be used to confirm nail psoriasis such as:
- Nail biopsy
- Dermoscopy
- Videodermoscopy
- Capillaroscopy
- Ultrasound
- Optical coherence tomography
- Confocal laser scanning microscopy
There is no cure for nail psoriasis, but these treatment methods are widely used to curb nail psoriasis from getting worse
Genital psoriasis
What Is Genital Psoriasis?
Psoriasis in the pubic area is called genital psoriasis.
Genital psoriasis can develop at any age and is common in both men and women.
(Young) children can also get psoriasis in the pubic area.
The occurrence of genital psoriasis is often underestimated. Research shows that about half of all people with psoriasis have had psoriasis in the pubic area.

Image courtesy pcds
What are the symptoms of genital psoriasis?
- Skin redness, ranging from pale pink to bright red, is the paramount sign of genital psoriasis.
- The skin may flake, but this is often minimal.
- The patches vary in size and can occur anywhere in the pubic area:
- Women: the mound of Venus, labia majora and minora, groin fold, thigh fold, skin towards and around the anus.
- Men: base of the penis, penis, glans, scrotum, groin crease, thigh crease, skin towards and around the anus.
The complaints of patients with genital psoriasis are precarious. Most people with genital psoriasis itch. The skin can also hurt or feel like it’s burning.
The severity of these complaints can vary from minimal to very serious. Chaps and cracks can form in the skin which can be very painful, especially when going to the toilet.
As with other forms of psoriasis affecting other parts of the body, genital psoriasis can worsen due to, for example, skin damage, illness, and psychological stress.
Logically, genital complaints in psoriasis patients can also indicate a condition other than genital psoriasis, for example, a fungal infection, a sexually transmitted disease (STD), or another skin disease.
When in doubt it is important to have yourself examined by a doctor.
How is genital psoriasis diagnosed?
The diagnosis of genital psoriasis can usually be made by a dermatologist by a visual inspection of the skin in the genital area.
In some cases, some skin flakes will be scraped off or a piece of skin will be removed under local anesthetic for microscopic examination (a biopsy).
Because of the thin skin in the genital area, treating genital psoriasis may prove to be challenging.
How Is Psoriasis Treated?
There is no psoriasis cure. There are, however, psoriasis treatments that can temporarily reduce the complaints.
What can be done about psoriasis?
Until now, there is no treatment to cure psoriasis. Still, a lot can be done about the symptoms of psoriasis. The complaints almost always improve with treatment, or they disappear completely. They generally return after a while once treatment has ended.
Who treats you?
In most cases, your doctor will prescribe treatment. In certain situations, he or she will refer you to a specialist.
You can also do a number of things yourself to relieve your symptoms.
- The general practitioner
The general practitioner gives the local treatments to people with psoriasis. The treatment is determined in consultation with you.
- The dermatologist (skin doctor) or nurse specialist
Sometimes the doctor will refer you to a skin specialist. This happens in about a quarter of people with psoriasis who visit their doctor. You may be treated by a nurse specialist. He or she specializes in the treatment of psoriasis and may take over certain tasks from the doctor.
- The rheumatologist
If you have psoriatic arthritis, you will be treated not only by a dermatologist but also by a rheumatologist.
To treat or not to treat?
Psoriasis is neither contagious nor life-threatening. Treatment is therefore not strictly always necessary.
You decide whether a treatment is acceptable for you (and your family) and how much time you want to spend on it.
The treatment depends on your complaints, the extent of the spots, and how much they bother you. Everyone has their own psoriasis, it is sometimes said.
Certain forms of psoriasis, such as psoriasis on the hands and feet, will almost always be treated because they are bothersome.
In other cases, it mainly depends on what you want.
Sometimes it is enough to take good care of your skin with neutral ointments and creams. The doctor will inform you about the options so that you can make a decision in consultation with your doctor.
Because psoriasis is chronic, you will often receive lifelong guidance from the doctor.
The reasons to treat or not to treat depend on your personal situation.
Some of the considerations for psoriasis treatment include:
- Social complaints: psoriasis limits you in your daily life. You are ashamed of the spots and the flakes, you avoid sports and swimming, you do not dare to go to the hairdresser, etc.
- Physical discomfort: you feel itching, pain, or fatigue.
- The psoriasis is extensive: much of the body is affected.
- The psoriasis is on unpleasant spots: your hands or feet, in skin folds, and so on. Genital psoriasis affects a person’s sex life.
Reasons not to treat:
- You are not or not very bothered by the spots.
- The drugs can have side effects that are more serious than the complaints.
- The complaints can diminish by themselves, for example, because you have less stress.
Psoriasis treatment methods
The main treatments are topical therapy, light therapy, and systemic therapy. In addition to these treatments, you can opt for courses, an alternative treatment method, or talk therapy.
- Topical therapy
There are a variety of ointments, creams, and lotions that you can put on the psoriasis patches. This is called topical therapy since you use the product directly in the areas where you have complaints.
Topical therapy is the most commonly used treatment for psoriasis. The treatment is effective and has few side effects. A doctor will almost always prescribe a cream or ointment.
You usually first get a cream or ointment with corticosteroids (steroids) or a vitamin D derivative. A combination is also possible. If these products do not work effectively enough, there are other options.
The active ingredients come in many forms: ointment, cream, emulsion, lotion, or gel. Whether you get a lotion, ointment or other means for the skin depends on where the spots are, how extensive they are and which formulation you yourself prefer.
- Light therapy
If lubrication alone does not help enough, a dermatologist can prescribe a light cure. Some people receive direct light therapy because the areas are so extensive that smearing is almost impossible.
Light therapy inhibits inflammation in the skin. You can be treated with UV-A or UV-B light. These components are also present in sunlight, but the therapy is not an ordinary tanning bed treatment. The type you get depends on the shape and severity of psoriasis.
You often have to visit an outpatient clinic or a day treatment center two to three times a week for light therapy. The therapy is applied in a lighting booth.
The psoriasis spots are illuminated with special lamps. In some cases, you will combine light therapy with medicines, special baths, and ointments.
Light therapy often works well, but cannot be given for too long at a time. Too much exposure accelerates the aging of the skin. It is preferable not to prescribe light therapy to children.
- Systemic Therapy
Sometimes a dermatologist will prescribe medicines to be taken, injected under the skin or into the bloodstream, or administered via an IV (intravenous) drip.
You will receive this treatment for severe forms of psoriasis when other treatments do not help enough.
Just like the local medicines, the drugs suppress the immune system and/or inhibit inflammatory reactions. These drugs can have a variety of side effects.
- Controls
When the doctor prescribes local therapy, he or she will also arrange a follow-up consultation with you. You will also return to the dermatologist for a check-up after a few weeks.
During this check-up, it is checked whether the treatment is working properly and whether you suffer from side effects.
At this appointment, you can indicate how satisfied you are with the treatment method and the results. It will then be decided in consultation whether you will continue with the drug in question or try another treatment. If the treatment is successful, you will only get a check-up if you think it is necessary.
- Other treatment methods
All treatments combat the symptoms (complaints) of psoriasis. Treatments cannot cure psoriasis.
In addition, all medications have possible side effects. Many people with psoriasis also try other treatment methods.
- Natural treatments
Natural cures are popular among people with psoriasis. You work intensively for a certain period of time on the recovery of the skin.
The most famous cure for psoriasis is the Dead Sea cure, which uses the beneficial effects of sun and saltwater on the skin. There are also spa centers where treatments usually consist of bathing in beneficial (spring) water, bathing with nibble fish, light therapy, and ointment therapy.
An advantage of these treatments is that there are few side effects. Moreover, the relaxation of a few weeks away can also help against the complaints.
A disadvantage is that a cure often costs a lot of money and time and the benefit of the above treatments has not always been demonstrated.
- Alternative treatment methods
Many people with psoriasis also use alternative treatments.
An alternative medicine practitioner does not only look at the skin condition but at the whole person (‘holistic approach’). Especially when a condition cannot be cured by doctors, such an approach appeals to many people.
Note: there are no alternative treatments that can cure psoriasis.
Many people use an alternative treatment. They usually do this in addition to – not instead of – normal treatment.
Especially people with a chronic condition are often satisfied with it. They report that alternative treatments can relieve certain complaints, such as pain and fatigue, and that the treatment generally makes them feel better and stronger.
However, the effect of the treatments has not been scientifically proven and is based more on the experience of patients and practitioners.
In general, there is little cooperation between mainstream and alternative medicine. It does sometimes happen that ‘a combination of’ is offered, for example, a general practitioner who is also a homeopath.
What can you do to lessen psoriasis complaints?
We already discussed how some things can make psoriasis worse such as stress, infections, certain medications, etc.
There are other things, however, that have a positive effect in the sense that they can lessen the complaints, such as sunlight, saltwater, relaxation, and proper skincare.
By keeping the skin supple and living a healthy lifestyle, the psoriasis symptoms can be less severe.
Psoriasis skincare
Take care of your skin. The skin has various functions, such as protecting the body against external influences and regulating the temperature and moisture balance. Good skincare is therefore important.
Water and soap dry out the skin. Not too hot water and not showering too long will limit the damage to your skin.
Ointments and creams. A good basic ointment or cream keeps the skin supple and prevents it from drying out. The choice of a good care product depends on the condition and type of your skin and what you like yourself.
Hair and nails. Try to avoid damage to the skin as much as possible. For example, wash your hair with mild products and cut your nails short to avoid scratching.
Sunbathe and swim. Sunbathing can be good for the skin. Properly dosed UV radiation has an anti-inflammatory effect on the skin.
Healthy living
- Lifestyle. A healthy lifestyle can sometimes reduce psoriasis symptoms. Healthy living means: eating healthy, getting enough exercise, losing weight if necessary and quitting smoking, and learning to deal with stress properly.
- Quit smoking. Smoking can have a bad influence on psoriasis symptoms. There are countless other reasons to quit smoking: it costs a lot of money, it will give you a bad condition, your skin will turn gray, you have an increased risk of all kinds of serious ailments. Successful quitting usually works best if you let yourself be guided.
- Healthy food. There are a number of rules about healthy eating: eat a varied diet, not too much, little saturated fat, lots of vegetables, fruit and bread. Also, make sure the food is safe.
- Move more. In order to maintain or build up good health, it is necessary to exercise at least half an hour ‘moderately intensively’ at five, but preferably on all days of the week. Listen to your body and gradually build up the movement no matter what your goal is.
- Lose weight. Obesity is very harmful to health. Therefore, it is advisable to lose weight in a healthy way. You can do this by making permanent changes to your eating and exercise habits and, if necessary, by following an energy-restricted diet.
- Deal with stress. Stress in itself is not unhealthy, but it can cause damage in the long run. It is therefore advisable to deal with excessive stress.
Conclusion
Think, feel, act. Psoriasis can lead to a negative self-image. This affects your mood and behavior.
Breaking negative thinking. If you can manage to break through negative thinking, you will certainly not have all positive thoughts left, and that is not the intention either.
Life is not only negative, but it is not only positive either. This applies to almost everything: negative and positive sides are intertwined, they are both part of it.
In fact, it can be said: by breaking through negative thinking you will think more sensibly, and your thoughts will then better reflect what your life really is like.