Choosing the best pustular psoriasis treatment option is largely determined by the type of pustular psoriasis a person suffers from.

Page Contents
What is pustular psoriasis?
Pustular psoriasis is a rare subspecies of psoriasis that manifests itself as superficial, flat pustules on various parts of the skin.
The pus in the lesions consists mainly of defense cells of the immune system, the neutrophils. Unlike pus, which forms after bacterial infections, the pus in the lesions of pustular psoriasis is not infectious.
While around 90 percent of psoriasis patients suffer from common psoriasis, psoriasis Vulgaris, pustular psoriasis affects less than five percent of those affected.
Pustular psoriasis can be recognized by the grouped pus lesions that gather around a reddened halo.
Pustular psoriasis can, depending on the form of the disease, be accompanied by fever and a feeling of severe illness. The patients feel exhausted.
Since pustular psoriasis can be a life-threatening disease, patients should be in constant contact with an experienced dermatologist.
Types of pustular psoriasis
There are 3 main pustular psoriasis types defined by the area of the body affected:
- Palmoplantar pustulosis psoriasis (PPP) – palms of the hands and/or the soles of feet
- Acropustulosis of infancy (severe itchy rash appears on hands and feet of infants)
- Generalized or Von Zumbusch pustular psoriasis (large areas of the skin affected by pus-filled blisters)
Sub-types of generalized pustular psoriasis:
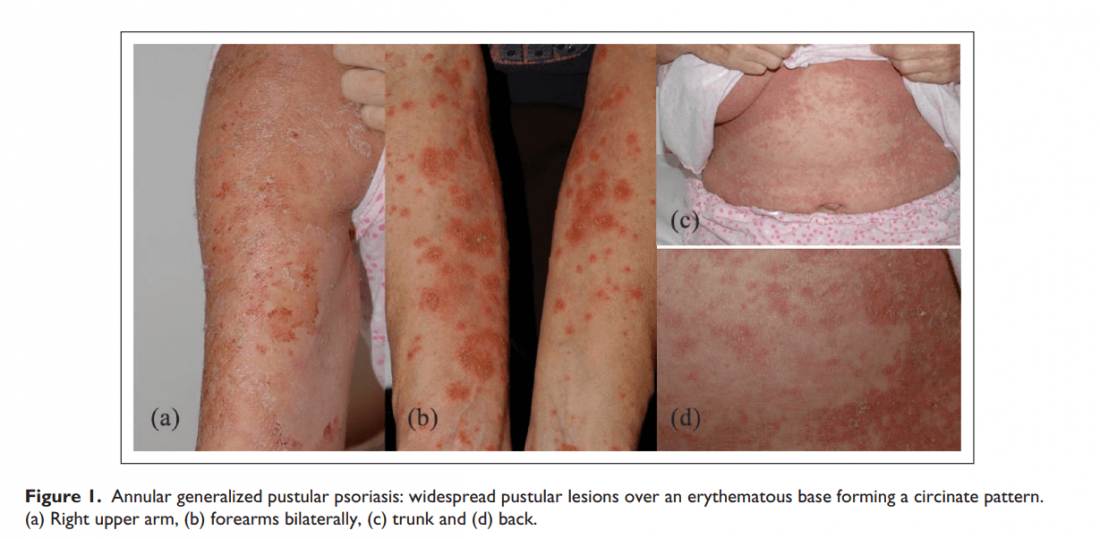
- Annular Pustular Psoriasis (APP) – a rare form of psoriasis with clinically annular ring-shaped configuration
- Impetigo herpetiformis (aka generalized Pustular Psoriasis of Pregnancy – PPP) – only develop in pregnant women, and usually in the 3rd trimester
Subtypes of pustular psoriasis
Depending on the appearance of the pus-filled lesions, a distinction is made between four subtypes of pustular psoriasis. In two forms, the pustular vesicles appear all over the body (generalized forms), while the other two forms are limited to the feet and hands (localized forms: palmoplantar and acropustulosis).
- Generalized pustular psoriasis:
If the lesions appear all over the body, three subspecies of pustular psoriasis can be considered:
Von Zumbusch type: Those affected suddenly develop large pustules all over their bodies. These flow together and form so-called pus lakes. At the same time, a high fever occurs, and the risk of edema, water retention inside the body, increases. Treatment in a dermatology clinic is essential.
Circular type (annular): The pus-filled pustules appear around a reddening of the skin. The confluence of the bubbles creates patterns that change quickly.
Generalized Pustular Psoriasis of Pregnancy – PPP: Particularly difficult during pregnancy. Affected women often have chills, fever, or diarrhea.
The disease can impair the functioning of the placenta so that the baby is not supplied with sufficient nutrients (placental insufficiency).
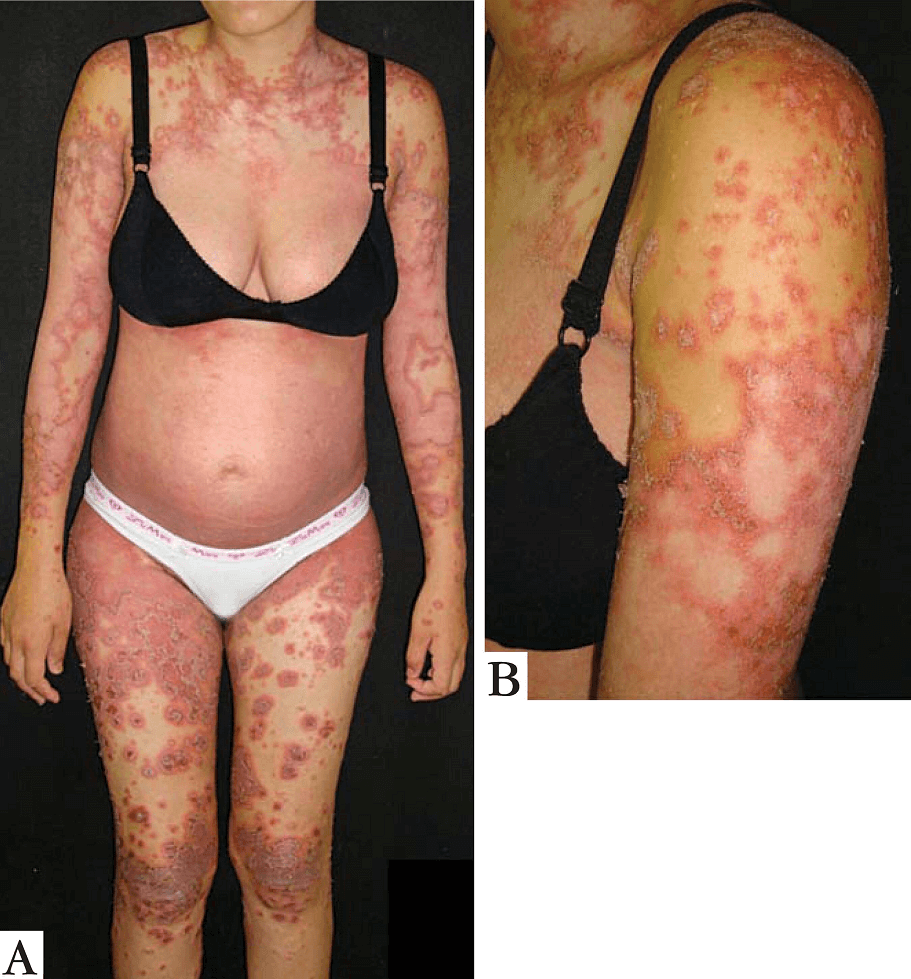
FIGURE A – 27 weeks into the first pregnancy. B- Detail of lesions on arm. Pustules on the periphery of the lesions. (Picture courtesy https://www.scielo.br/)
- Localized: affects fingers and feet:
When the pus-filled lesions are limited to the feet and hands, the doctor speaks of localized pustular psoriasis. The two localized forms are very rare.
A distinction is made between 1) Andrews-Barber type, which occurs on the palms and soles of the feet, and 2) Acrodermatitis continua of Hallopeau (ACH) type, which only appears on the tips of toes and fingers.
Andrews-Barber type (palmoplantar pustulosis): The pustules form symmetrically on the palms of the hands and soles of the feet. Due to the mechanical stress on the hands and feet, the pustules adhere to the skin in coarse scales.
Newer pustules are yellowish in color, older ones are more brownish due to crust formation and desiccation. Smokers are, particularly at risk.
Acrodermatitis continua of Hallopeau (ACH): This type is identified by eruptions that start in the finger and toe tips.

Pustular Psoriasis Treatment
Pustular psoriasis treatment is based on the individual disease type and the treatment course is developed in cooperation with a dermatologist. Although pustular psoriasis, like all types of psoriasis, cannot be cured, the symptoms can be alleviated.
Treating palmoplantar psoriasis
An effective proven treatment does not exist for palmoplantar pustulosis. The condition is difficult to treat because the symptoms come and go in many patients.
However, it is possible to relieve the symptoms. Some common treatment options are:
1.Topical (applied to the skin) steroid creams or ointments
Corticosteroid ointments with or without a vitamin D preparation are the topical agents of choice for this formulation. Often the ointment is applied under a special wound dressing for a few days and then repeated again.

2. Light therapy
When psoriasis only affects the palms and soles of the feet, topical PUVA is usually prescribed. Only these areas are illuminated with UVA rays. The hands and feet must be bathed in or rubbed with a special gel containing psoralens for about 10 minutes before exposure. This will make the UVA lighting work better.
3. Systemic means
The doctor may use medication to reduce the activity of the immune system such as methotrexate, cyclosporine, fumaric acid, and apremilast can be used when topical treatments do not work. Biologicals are also effective, and certainly a good option if the psoriasis is all over the body and does not respond to all of the above agents.
Complaints do not always diminish during a treatment; sometimes the patient has to test multiple treatments or a combination of treatments may be required before the skin lesions and additional signs diminish.
Andrews-Barber and Hallopeau types can often be treated well locally with ointments, creams, or gels. Proven ingredients of local therapy are methotrexate or cyclosporin A, as they keep the inflammation in check.
Prognosis
The condition is chronic and flare-ups do occur. The patient, therefore, has calmer periods followed by new blistering of the hands or feet. However, not all patients experience flare-ups because in some patients only one episode of symptoms occurs and then do not return. Typically, lifestyle changes and some preventative steps will help slow and less severe flare-ups.
Complications
Blisters, ulcers, and other skin lesions on the hands and/or feet sometimes cause complications that lead to a reduced quality of life such as:
Scratching due to the intense itching of the hands and feet
Problems walking or taking part in other activities that require movement
Sleep interruption due to the pain
How to prevent palmoplantar psoriasis flare-ups
By taking some measures, it is possible to reduce the severity and frequency of flare-ups. This is possible by:
- Avoid bath foam and shower gels
- Keep the affected skin areas clean
- Rest the hands and feet often
- Protect the skin from chemicals, water, and possible irritants. Use perfume-free hypoallergenic washing products that irritate as little as possible
- Avoid injury to the skin. Use vinyl gloves for wet work and cotton or silver-containing bandage gloves for dry work or during sleep. This will protect your hands against further irritation and damage. The prescribed ointment can also work better at night
- Use moisturizing soap
- For the feet: use cotton or silver socks at night after applying the medicated ointment. This will prevent the ointment from getting on the bedding instead of your skin
- By moisturizing the spots daily with petroleum jelly and/or urea-containing ointment you can prevent cracks from forming
- Treat cracks by applying zinc ointment to it and cover with a Band-Aid
- Avoid shoes made of synthetic products
- Quit smoking

Treating Acropustulosis of Infancy
Read more about the symptoms of acropustulosis of infancy if not you’re familiar with it.
While acropustulosis is uncomfortable, it generally is not a serious skin condition.
To prevent scratching that may result in scars and/or damage to the skin, it is advised to put soft cotton socks and gloves on the baby’s feet and hands.
As the baby gets older, the flare-ups are bound to be less frequent, and also less serious.
Some children may need to be treated for infantile acropustulosis, but many will, however, not need any treatment.
Based on how serious the acropustulosis symptoms are, treatment may not require very strong medicine. Some of the treatment options generally prescribed are:
1.Oral antihistamine
For relief from the itchiness, a prescription for an oral antihistamine should suffice.
Histamine is a substance that is produced by the body itself. There are various causes that can cause the histamine level in your body to rise too much. The allergic reaction is caused by antibodies coming into contact with cells containing histamine and then releasing it. This can manifest itself in, for example, itching, a rash, a blocked nose, or asthmatic complaints.
It is not advised to treat infants with antihistamines unless prescribed by a medical practitioner as it has certain side effects which include sleepiness.
2. Topical Steroids
Topical steroids with moderate to high potency are usually the very first treatment recommended by doctors.
Topical steroids are available in ointment, cream, or solution form and are an anti-inflammatory medication applied directly to the skin. Application of the topical steroid is once to twice daily for a few days and can be as long as a few weeks.
It is imperative you follow the doctor’s guidance on how to administer the treatment. When topical steroids are used over long periods of time or incorrectly, they can cause side effects when too much is absorbed from the skin by your body.
Dry skin is sometimes caused by topical ointments. Use a moisturizing cream to restore the moisture once you completed the treatment as prescribed by your doctor.
3. Topical Ointments
Topical ointments containing a corticosteroid, such as betamethasone valerate (Betnovate) are usually prescribed to treat an acropustulosis rash. These ointments usually work very well to reduce skin inflammation and also bring relief from itchiness.
Dapsone (Aczone) is a potent antibiotic that is used topically to treat severe cases of acne. It may be used to treat severe instances of acropustulosis.
Topical ointment treatment will only be prescribed by a doctor in severe cases of infantile acropustulosis.
The infants will be closely monitored since these treatments pose a significant risk of side effects; some of which include an upset stomach, anemia, headaches, and a lot more serious, muscular weakness.
Keep in mind that acropustulosis is a skin condition that is only temporary; it tends to come and go. In most instances, flare-ups are bound to stop when the infant reaches the age of 3 years.
Flare-ups are much easier to manage by protecting the affected areas of the skin and using good medication.

Treating Generalized Pustular Psoriasis (Von Zumbusch)
As indicated earlier, Von Zumbusch psoriasis must be treated as a life-threatening disease by seeking urgent specialist medical care.
Treatment is administered in a healthcare facility such as a hospital where the treatment aims to:
- Stop any further loss of fluids
- Stabilize the body temperature
- Restore the imbalance in electrolytes
Treating affected areas with cool compresses and taking an oatmeal bath may assist in soothing the skin and allow for the dead skin to be removed.
In most cases, it is possible to deal with the acute attack with only topical steroids, after which systemic medications may be required for the longer term.
As a first choice is specifically mentioned Acitretin, an oral retinoid used only in severe cases of psoriasis, for instance, Von Zumbusch pustular psoriasis. Retinoid slows down the proliferation (reproduction) of skin cells thus helping to bring symptoms under control.
More serious cases may need to be treated with immunosuppressants (systemic) medications such as cyclosporine, infliximab, adalimumab, or methotrexate.
The safest approach is intensive local therapy. Wait until the waves of pustules have passed before starting with immune suppressants.
Stopping suddenly with oral steroids can bring about a recurrence of von Zumbusch psoriasis. You need to slowly decrease your intake of these medications and always under the supervision of your doctor. Consult with your doctor about the risks associated with oral steroids so you can understand how they affect you.
In the widespread forms of generalized pustular psoriasis, medication containing the active ingredient acitretin, which is related to vitamin A, often has to be taken over the long term.
How to Prevent Generalized Pustular Psoriasis
Considering the fact that very little about what causes generalized pustular psoriasis (Von Zumbusch) is known, prevention is hardly possible.
People who have had a flare-up, are more prone to a recurrence, and there are actually some steps they can take to prevent flare-ups:
- Quit smoking. Smoking has been found to be a major factor in getting Von Zumbusch psoriasis. While it may not necessarily bring about the disease, it does appear to heighten the risk of a flare-up exponentially.
- Reduce your alcohol consumption. Regular (non-light) beer generally increases the chance of getting psoriasis. If becoming a teetotaler is not an option, restrict your daily intake to 2-3 drinks and change to light beer, wine, etc.
- Avoid too much sun. Exposure to the sun is how we naturally get enough Vitamin D. Over-exposure, however, increases the risk of psoriasis. Spending 10 to 30 minutes in the sun daily is sufficient for our skin. Use sunscreen liberally and stay away from sunbeds.
- Manage your stress levels. Make sure you get exercise (swimming, walking, jogging, participate in a sport) and get enough sleep. Deep breathing exercises, visiting friends, laughing, aromatherapy, etc. are all ways to free your body of unnecessary stress.
Pustular Psoriasis Natural Treatment
Aloe Vera Gel: rich in vitamins and nutrients for all skin types. To perfectly complement the intense effects of aloe vera, the 100% pure aloe gel is packed with 200 active compounds, making the benefits limitless!
Soothing Hydration for the Skin: The moisturizing properties of our aloe vera gel penetrate deep into your skin and provide excellent hydration for clearer, healthier skin. It feels fresh and looks fresh and revitalized.
Conclusion
Corticosteroids (cortisone) for the treatment of pustular psoriasis have not proven effective! After stopping the drug, there is a relapse with increasing pustules and pus formation (rebound effect).
In addition to the medication prescribed by a doctor, many psoriasis patients also recommend taking home remedies such as aloe vera, which has an anti-inflammatory effect.