Meningitis is a serious and potentially life-threatening condition characterized by the inflammation of the protective membranes, known as meninges, that surround the brain and spinal cord. This inflammation can result from various causes, including infections, autoimmune diseases, and reactions to medications. While meningitis can affect individuals of all ages, it poses a significant risk to infants, young children, and those with weakened immune systems. Early recognition and treatment are crucial to preventing severe complications or death.
This article provides a comprehensive overview of meningitis, including its causes, symptoms, prevention strategies, and treatment options.
What is Meningitis?
Meningitis occurs when the meninges, the membranes that cover the brain and spinal cord, become inflamed. This inflammation can lead to swelling, which in turn can cause a range of symptoms and potentially serious complications. Meningitis can be categorized into several types based on its cause:
- Bacterial Meningitis:
- Cause: This is the most severe form of meningitis and is typically caused by bacterial infections. Common bacteria that can cause bacterial meningitis include Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Bacterial meningitis is a medical emergency and requires immediate treatment with antibiotics.
- Severity: Bacterial meningitis can be fatal if not treated promptly. Even with treatment, it can lead to long-term complications such as hearing loss, brain damage, and learning disabilities.
- Viral Meningitis:
- Cause: Viral infections, particularly those caused by enteroviruses, are the most common cause of viral meningitis. Other viruses, such as the herpes simplex virus, mumps virus, and West Nile virus, can also cause viral meningitis.
- Severity: Viral meningitis is generally less severe than bacterial meningitis and often resolves on its own without specific treatment. However, it can still cause significant discomfort and requires supportive care.
- Fungal Meningitis:
- Cause: Fungal meningitis is caused by fungal infections, such as Cryptococcus or Histoplasma. It is rare and typically affects individuals with compromised immune systems, such as those with HIV/AIDS or cancer.
- Severity: Fungal meningitis is serious and requires antifungal treatment. It can be life-threatening, especially in immunocompromised individuals.
- Parasitic Meningitis:
- Cause: This rare form of meningitis is caused by parasites, such as Naegleria fowleri, which can enter the body through contaminated water. Parasitic meningitis is often associated with swimming in warm freshwater.
- Severity: Parasitic meningitis is typically very severe and often fatal.
- Non-Infectious Meningitis:
- Cause: Non-infectious meningitis can result from causes other than infections, such as autoimmune diseases (e.g., lupus), certain medications, or cancers that affect the meninges.
- Severity: The severity of non-infectious meningitis varies depending on the underlying cause and may require specific treatment to address the source of inflammation.
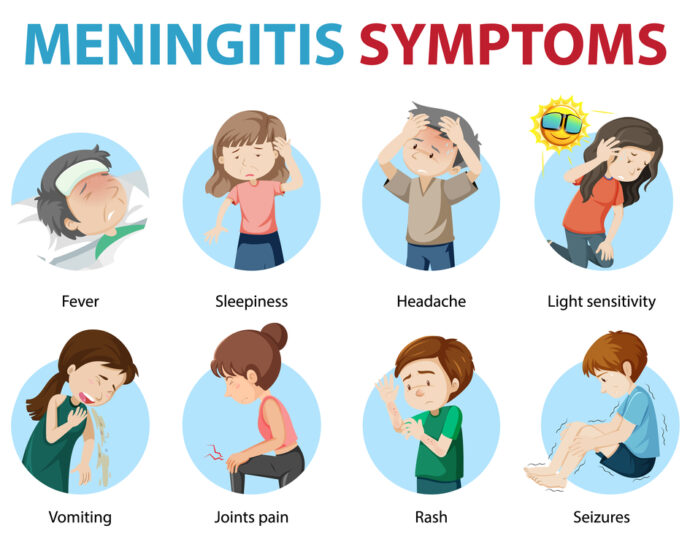
Recognizing the Symptoms of Meningitis
The symptoms of meningitis can vary depending on the type and severity of the infection, as well as the age of the individual. However, some common symptoms to be aware of include:
- High Fever: A sudden onset of a high fever is a common symptom of meningitis, particularly in bacterial cases.
- Severe Headache: One of the hallmark symptoms, the headache associated with meningitis is often described as intense and persistent.
- Stiff Neck: Neck stiffness, particularly when attempting to touch the chin to the chest, is a classic symptom of meningitis.
- Nausea and Vomiting: Many individuals with meningitis experience nausea and vomiting.
- Sensitivity to Light (Photophobia): Bright lights may cause discomfort or worsen the headache in individuals with meningitis.
- Confusion or Altered Mental Status: Meningitis can lead to confusion, difficulty concentrating, drowsiness, or even seizures.
- Rash: In cases of bacterial meningitis caused by Neisseria meningitidis, a distinctive rash may develop. This rash may start as small, red or purple spots and can progress to larger patches.
- Fatigue and Lethargy: Individuals with meningitis often feel extremely tired or lethargic.
- Seizures: In severe cases, meningitis can lead to seizures, particularly if there is swelling of the brain.
- Cold Hands and Feet: Poor circulation, resulting from the body’s response to infection, may cause cold extremities.
In infants and young children, symptoms may be more subtle and can include irritability, poor feeding, a bulging fontanel (soft spot on the head), and unusual crying.
Diagnosing Meningitis
Diagnosing meningitis typically involves a combination of clinical evaluation, laboratory tests, and imaging studies:
- Lumbar Puncture (Spinal Tap): This is the definitive test for diagnosing meningitis. A small amount of cerebrospinal fluid (CSF) is extracted from the spinal cord and analyzed for signs of infection or inflammation, such as the presence of bacteria, viruses, or white blood cells.
- Blood Tests: Blood tests can help identify the presence of infection, inflammation, and the specific bacteria or virus causing the meningitis.
- Imaging Studies: In some cases, imaging studies such as a CT scan or MRI may be performed to assess for complications such as brain swelling or abscesses.
- Cultures and PCR Tests: Cultures of CSF or blood, and polymerase chain reaction (PCR) tests, can help identify the specific pathogen responsible for the infection.
Treatment Options for Meningitis
The treatment for meningitis depends on the underlying cause:
- Bacterial Meningitis:
- Antibiotics: Immediate treatment with intravenous antibiotics is critical for bacterial meningitis. The choice of antibiotic depends on the type of bacteria causing the infection.
- Corticosteroids: In some cases, corticosteroids may be administered to reduce inflammation and prevent complications.
- Viral Meningitis:
- Supportive Care: Since viral meningitis typically resolves on its own, treatment focuses on relieving symptoms. This may include rest, hydration, and over-the-counter pain relievers.
- Antiviral Medications: In certain cases, such as herpes simplex virus meningitis, antiviral medications may be prescribed.
- Fungal Meningitis:
- Antifungal Medications: Treatment involves the use of antifungal drugs, often administered over an extended period.
- Parasitic Meningitis:
- Antiparasitic Treatment: Treatment options are limited, and early diagnosis is critical. Supportive care is often the primary approach.
- Non-Infectious Meningitis:
- Treatment of Underlying Cause: Addressing the underlying condition, such as an autoimmune disease, is essential. This may involve corticosteroids or other immunosuppressive therapies.
Preventing Meningitis
Prevention strategies vary depending on the type of meningitis:
- Vaccination:
- Meningococcal Vaccine: Vaccination against Neisseria meningitidis is recommended for adolescents, college students, and travelers to certain regions.
- Pneumococcal Vaccine: This vaccine protects against Streptococcus pneumoniae, a common cause of bacterial meningitis.
- Haemophilus Influenzae Type B (Hib) Vaccine: Hib vaccination is part of the routine childhood immunization schedule and has significantly reduced cases of bacterial meningitis.
- Good Hygiene Practices:
- Handwashing: Regular handwashing with soap and water can help prevent the spread of viruses and bacteria that cause meningitis.
- Avoid Sharing Personal Items: Avoid sharing drinks, utensils, or other personal items that can transmit germs.
- Avoiding Close Contact with Infected Individuals:
- If someone in your household or community has bacterial meningitis, taking precautions such as prophylactic antibiotics (for close contacts) may be necessary.
- Prompt Treatment of Infections:
- Treating respiratory infections and ear infections promptly can reduce the risk of these infections spreading to the meninges.
Conclusion
Meningitis is a serious and potentially life-threatening condition that requires prompt recognition and treatment. Understanding the different types of meningitis, their causes, symptoms, and treatment options is crucial for preventing severe complications. Vaccination, good hygiene, and early medical intervention are key strategies in reducing the risk of meningitis. By staying informed and vigilant, individuals can protect themselves and their loved ones from this dangerous condition.
READ MORE: Understanding the Link Between Gut Health and Systemic Inflammation
Sources:
https://www.who.int/news-room/fact-sheets/detail/meningitis#:~:text=Meningitis%20is%20the%20inflammation%20of,transmitted%20from%20person%20to%20person.
https://my.clevelandclinic.org/health/diseases/14600-meningitis
https://www.webmd.com/children/understanding-meningitis-basics
https://www.cdc.gov/meningitis/about/index.html