Dermatitis herpetiformis symptoms may differ from person to person. The most common dermatitis herpetiformis symptoms manifest in the skin, oral, and gastrointestinal problems relating to gluten sensitivity or allergy.
Page Contents
What is Herpetiform Dermatitis (HD)?
Dermatitis herpetiformis is largely an uncommon, chronic skin disorder also known as Duhring-Brocq disease, Brocq-Duhring disease, Duhring disease, dermatitis multiformis, or DH.
It is characterized by the formation of groups of blisters on various parts of the body that is accompanied by severe itching. Many patients with HD suffer from celiac disease, an inflammatory autoimmune disease of the small intestines.
Dermatitis herpetiformis can start in people of any age, but it generally affects people in the 30-40 age group. Where oral and genital areas are concerned, men tend to be more prone than women to experience problems.
People who have close relatives suffering from DH or celiac disease have a very slight risk of also getting the disease.
Since the disease is chronic, symptoms can keep coming up. In many cases, the intensity of the symptoms diminishes over the years.
Dermatitis herpetiformis is not contagious.
Causes of Dermatitis Herpetiformis
The disease is triggered when gluten is consumed. People who suffer from this skin condition should definitely be tested for celiac disease, as these two diseases are associated with each other.
A genetic predisposition cannot be ruled out.
Celiac disease, also known as gluten-induced enteropathy, is an intolerance to the gluten found in various types of grain.
The consumption of gluten causes chronic inflammation of the mucous membrane in the small intestine. The inflammation subsequently gives rise to tiredness, diarrhea, weight loss, and discomfort in the abdominal region.
This hypersensitivity reaction to gluten lasts for life. Dermatitis herpetiformis is the skin manifestation of celiac disease.

Dermatitis Herpetiformis Symptoms
Skin problems:
Skin problems are the most telling sign of dermatitis herpetiformis.
In the beginning, most sufferers of dermatitis herpetiformis develop skin lesions that are red and raised and occur in groups. Patients complain of severe itching of the skin and burning blisters on the affected areas. The urge to scratch becomes almost unbearable but is strongly advised against as the skin may break and give rise to infections that will exacerbate the condition.
Blisters filled with clear liquid gradually form on the reddened areas of the skin. The nodules on the surface of the skin are a few millimeters wide and develop into blisters characteristic of the skin disease after about seven to ten days. These can spread to neighboring skin tissue and form crusts that are quick to scratch off. Healing takes place within a few days. The resultant purple marks may remain for weeks before disappearing though.
Oral problems:
Tooth enamel problems may develop. Most common are discoloration, horizontal grooves, and pitting. Canker sores are rarely experienced.
Gastrointestinal problems:
Dermatitis herpetiformis is a skin manifestation of celiac disease. It is the result of gluten ingestion to which almost all celiac disease patients are allergic.
Celiac disease causes inflammation and damage to the small intestine. Most people suffering from dermatitis herpetiformis rarely have gastrointestinal issues when compared to those who have celiac disease. Dermatitis herpetiformis patients may, however, experience symptoms such as cramping, bloating, constipation, diarrhea, and pain.

Dermatitis Herpetiformis Diagnosis
Due to the rather unspecific symptoms, especially at the beginning of the disease, dermatitis herpetiformis is often recognized late. In order to establish a diagnosis, diseases that have similar symptoms must first be ruled out.
This disease describes an inflammation of the dermis. To confirm the diagnosis of dermatitis herpetiformis, a skin biopsy is done. The tissue removed for this is examined under a microscope in a laboratory.
In order to be able to make the diagnosis with certainty, evidence of so-called granular IgA deposits is necessary. This is done using an immunofluorescent stain.
Since many patients who suffer from Duhring’s disease also have celiac disease, a diagnosis of this clinical picture must also be carried out. To do this, blood tests are performed. Celiac disease antibodies that the blood is tested for are anti-tissue transglutaminase and anti-endomysial antibodies.
Also, a biopsy of the small intestine may be performed to confirm the diagnosis. Most patients suffering from Duhring’s disease show a rather harmless course of celiac disease. However, a few may experience massive fatty stools, osteoporosis, and vitamin deficiencies.
When should you go to the doctor?
In the case of hives-like rashes and other signs of dermatitis herpetiformis, a visit to your family doctor is recommended.
Reddening of the skin, severe itching, and blisters are also symptoms that indicate a serious skin disease and must be investigated accordingly. If swelling and abscesses develop as a result of incorrect or inadequate treatment, it is best to go to the nearest clinic. This is especially true if the bubbles fill with liquid or become encrusted.
In the case of a chronic course, regular visits to the doctor are indicated, which is why the disease is best diagnosed and treated at an early stage. Dermatitis herpetiformis is particularly common after a tumor disease, infection, and contact with iodine.
If these factors apply to you, you should consult a doctor immediately with the symptoms mentioned. In addition to the family doctor, the dermatologist or a specialist in internal medicine can also be contacted.
Dermatitis Herpetiformis Treatment
At this time, no cure for dermatitis herpetiformis exists. There are, fortunately, medications that can bring welcome relief from the itching and bumps associated with dermatitis herpetiformis.
Medication
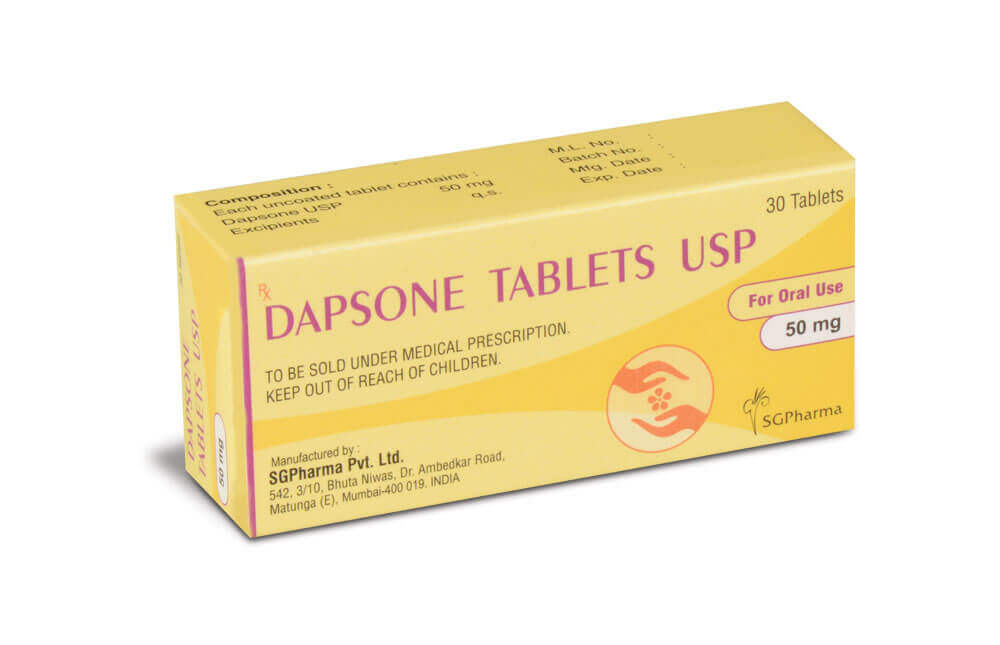
The itchy regions of the skin are usually treated with sulfone dapsone, an oral antibiotic. As a rule, most patients get relief from dermatitis herpetiformis symptoms within an hour of taking this medicine and typically not more than 48 hours.
To prevent the skin condition from forming again, patients may need to continue taking dapsone for a couple of years. Dapsone can have side effects and subsequently requires regular monitoring and testing.
Other medications which are less effective may be prescribed when dapsone either has adverse effects on a patient or does not control the dermatitis herpetiformis symptoms.
These alternatives are sulfasalazine, sulfamethoxypyridazine, or sulfapyridine. Side effects with these medications may also occur and include drug reactions, proteinuria (presence of abnormal quantities of protein in the urine), crystalluria (presence of crystals in the urine indicating renal irritation), and hemolytic anemia (red blood cells are destroyed faster than they can be made).
The affected skin areas and the itching can also be treated with topical ointments or lotions. In some cases, short-term treatment with cortisone-induced preparations is prescribed. Long-term special care of the skin is not necessary for dermatitis herpetiformis. Typically these topicals include betamethasone valerate or dipropionate, or the very potent clobetasol propionate.
Diet
Following a gluten-free diet will take a few months to yield results, and on its own, not the best treatment if you wish to get rid of your dermatitis herpetiformis symptoms.
Even so, going gluten-free can help bring some relief from dermatitis herpetiformis symptoms and benefit your health in general. It helps as follows:
Reducing the need for medication to control the skin condition.
Reducing the risk of developing other autoimmune diseases.
Reducing the risk of intestinal lymphoma.
Improving any gluten-sensitive intestinal disease.
Enhancing nutrition and bone density. Source
Iodine (an ingredient commonly found in salt) can aggravate the disease, foods rich in iodine should therefore be avoided, especially in the first month after diagnosis was made.
Since in most cases the celiac disease is the basis of dermatitis herpetiformis developing, dermatitis herpetiformis must be treated with the same therapy used to treat celiac disease. For those affected, this means that they have to do without the adhesive protein gluten for the rest of their life. Even the smallest amounts can drastically worsen the course of the disease.

Gastrointestinal symptoms can be alleviated on average between 3 and 6 months with a gluten-free diet. This is much quicker than the skin rash associated with a gluten allergy. A period of between 1 and 2 years may be needed to resolve skin rashes. Once the patient digests gluten again, the rash will recur.
Gluten is found in certain types of grain. These include, but are not limited to wheat, rye, barley, and commercial oats. Products made from these products such as couscous or pasta must also be eliminated from your diet. Corn, millet, rice, quinoa, soy, and buckwheat are expressly permitted. Products that do not contain any gluten are labeled with the addition “gluten-free” and can be consumed without hesitation.
Should flare-ups of dermatitis herpetiformis symptoms continue in spite of a patient going gluten-free and medication, iodine may need to be cut out from their diet completely.
Complications of Dermatitis Herpetiformis
Dermatitis herpetiformis is a rarely occurring incurable autoimmune skin disease. and is associated with other autoimmune diseases such as vitiligo, myasthenia gravis, rheumatoid arthritis, hypothyroidism, type 1 diabetes mellitus, and Sjogren’s syndrome (source)
Left untreated, the constant inflammation in the intestines due to gluten intolerance poses a higher risk of developing intestinal cancer.
Dermatitis herpetiformis begins with reddening of the skin. If the person concerned ignores the symptom or treats it incorrectly on their own initiative, painful swellings and unpleasant itching develop.
Other conditions which may also affect dermatitis herpetiformis sufferers, particularly when celiac disease is the cause include
- heart problems such as pericarditis and cardiomyopathy
- neurological problems relating to ataxia, epilepsy, and polyneuropathy
- fatty liver (results in abnormal liver function tests
- miscarriages (spontaneous abortions)
- dental problems (thin enamel)
With timely medical clarification, complications can be largely ruled out. A lifelong gluten-free diet is recommended in medical therapy.
Dermatitis Herpetiformis Outlook
With a consistent change in diet, patients with dermatitis herpetiformis have a good prognosis. In many cases, further medical care is usually not necessary. In the case of more severe symptoms, herbs help to relieve the changes in the skin or the itching. However, these are associated with side effects. Regular blood tests are therefore advisable in order not to trigger any further illnesses.
The patient can achieve lifelong freedom from dermatitis herpetiformis symptoms on their own initiative. To do this, check your food intake. All food must be gluten-free to get a good prognosis. In order to have a favorable healing prospect, no product may be consumed that contains even the smallest amounts of gluten. The body needs a few months to a year to be completely gluten-free for recovery.
Dermatitis herpetiformis symptoms flare-ups occur soon after gluten has been consumed. Therefore, there is always the risk in the course of life of experiencing a recurrence of the symptoms. There is an increased risk, especially when eating food in restaurants.
Without giving up gluten, the patient can fall victim to a chronic disease process. The general state of health is weakened and the susceptibility to disease is greatly increased. The quality of life decreases and health conditions become much more difficult in everyday life.
Dermatitis Herpetiformis Prevention
Prevention of the disease is only possible to a limited extent. Since dermatitis herpetiformis is associated with celiac disease and with high exposure to iodine, it is conceivable that a lifelong special diet could reduce the likelihood of this skin disease.
Aftercare
In the case of dermatitis herpetiformis, there are usually no special options or measures available for follow-up care. The person concerned is primarily dependent on full medical treatment in order to alleviate dermatitis herpetiformis symptoms and avoid further complications, as this cannot lead to independent healing.
Only through an early diagnosis and rapid treatment can a worsening of dermatitis herpetiformis symptoms be avoided. In most cases, dermatitis herpetiformis is treated with the help of medication, ointments, or creams. The person concerned should always pay attention to the instructions of the doctor and also pay attention to the intervals and dosage of the prescribed medication.
If you have any questions or are unclear, your doctor should always be contacted first.
If dermatitis herpetiformis symptoms do not go away within a few days, your doctor should definitely be consulted.
Since the illness can also lead to psychological upset or depression, intensive discussions with friends or with your own family are often very useful. In serious cases, however, professional advice from a psychologist is useful. As a rule, dermatitis herpetiformis does not reduce the patient’s life expectancy.
How to help yourself
Despite the difficult diagnosis, everyone can do a few things to improve their quality of life.
Self-discipline is important as the symptom of itching should not be indulged in. Scratching leads to open wounds that germs can penetrate. In addition, the skin damage increases. For their own sake, the person concerned should therefore make sure they use ointments if the itching is too strong and therefore not get tempted to scratch.
The skin changes lead to an optical flaw. This can reduce self-esteem. It is advisable to obtain comprehensive information about the disease and to find ways to maintain the patient’s aesthetic standards. Discussions and tips with other sick people or close relatives often help.
It can be beneficial to find out their attitude and perception of the skin changes. In many cases, the affected person experiences the visual flaw worse than those in their immediate environment. Changing cognitive patterns can therefore alleviate emotional distress.
Although it has not yet been adequately researched scientifically, it appears that a special diet may be beneficial for one’s own recovery. This must become a lifestyle that can contribute to a significant improvement in symptoms and an increase in their own well-being.