Endometriosis treatment options include pain medication, hormone therapy, and surgery. Unfortunately, at this time, there is no cure for this chronic condition.
/p>
Page Contents
What is Endometriosis?
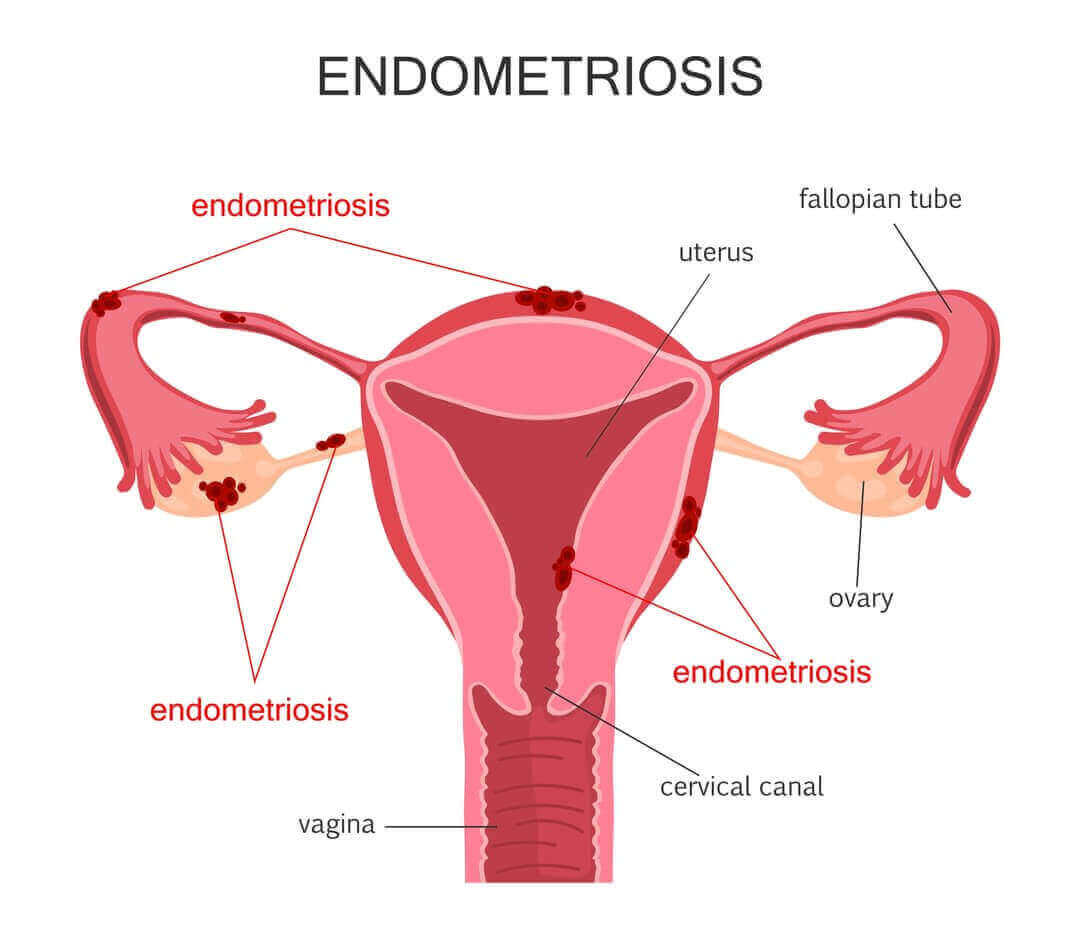
Endometriosis is a gynecological condition in which tissue cells that form the lining (endometrium) on the inside of the womb (uterus), also develop outside the uterus.
Endometriosis generally grows outside the womb on the ovaries, on the fallopian tubes, on the tissue that keeps the uterus in place, and on the outer surface of the uterus. Other areas where endometriosis may also develop are the vagina, vulva, bladder, rectum, bowel, or cervix.
In the US, between 2 and 10% of women between the ages of 25 and 40 are affected by the condition.
Causes of Endometriosis
The exact causes are not yet known. There are, however, a few theories that are studied by researchers that may help in explaining how endometriosis develops. Currently, however, there is no scientific proof of what causes endometriosis.
Some of the possible causes include:
Retrograde Menstruation. Known as retrograde menstrual flow, it is considered the most likely cause of endometriosis developing. Menstrual blood contains endometrial cells. Instead of the menstrual blood flowing out of the body, some of it flows through the fallopian tubes into another area of the body, such as the pelvic cavity.
The endometrial cells in the menstrual blood start to grow on the organs where the blood ended up and with every menstrual cycle these cells continue to bleed and grow thicker.
Genetic factors may also play a role. Since the disease of endometriosis runs in families, some women may genetically inherit endometriosis.
An immune system disease. When a person’s immune system is faulty it may be unable to detect and destroy the endometrial tissue which is busy growing outside of the womb (uterus). Women with endometriosis are more prone to disorders of the immune system.
Hormones. Wondering what hormones cause endometriosis? Estrogen. Estrogen dominance is what happens when estrogen and progesterone levels in a woman’s body are out of balance. Some of the high estrogen levels symptoms include, but are not limited to:
- Irregular menstrual periods
- Light or heavy Periods
- Aggravated PMS symptoms
- Bloating
- Irritability
Surgery. During surgery to the abdominal area, such as a Cesarean (C-section) or hysterectomy, endometrial tissue may be found to have attached itself to the abdominal incision.
Symptoms of Endometriosis
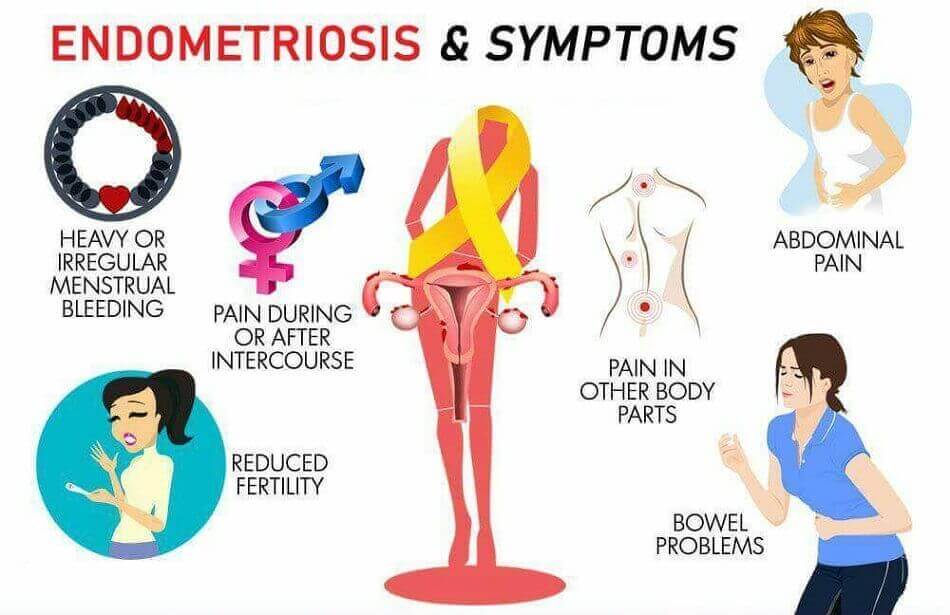
Pelvic pain. The main symptom of endometriosis that is most commonly experienced by women; linked to menstruation periods. Cramping generally affects many women during their menstrual periods. Women with endometriosis, however, experience pain much worse than is the norm.
Dysmenorrhea: the pain associated with menstruation. There are 2 types of dysmenorrhea, namely:
- primary: cramping experienced before and during periods
- secondary: pain may start a few days before the menstrual period, but progressively gets worse. As the menstrual period continues, pain continues to worsen and may only stop when the menstrual period ends.
Dyspareunia is painful intercourse. Described as persistent genital pain experienced before, during, and after intercourse.
Urination and bowel movement pain. Highly likely this pain is experienced during menstruation.
Infertility. Endometriosis is oftentimes diagnosed when people start looking for infertility treatment.
Other symptoms sometimes experienced by some women with endometriosis include chronic fatigue, heavy or irregular menstruation, lower back pain, or lower abdominal pain.
Stages of Endometriosis
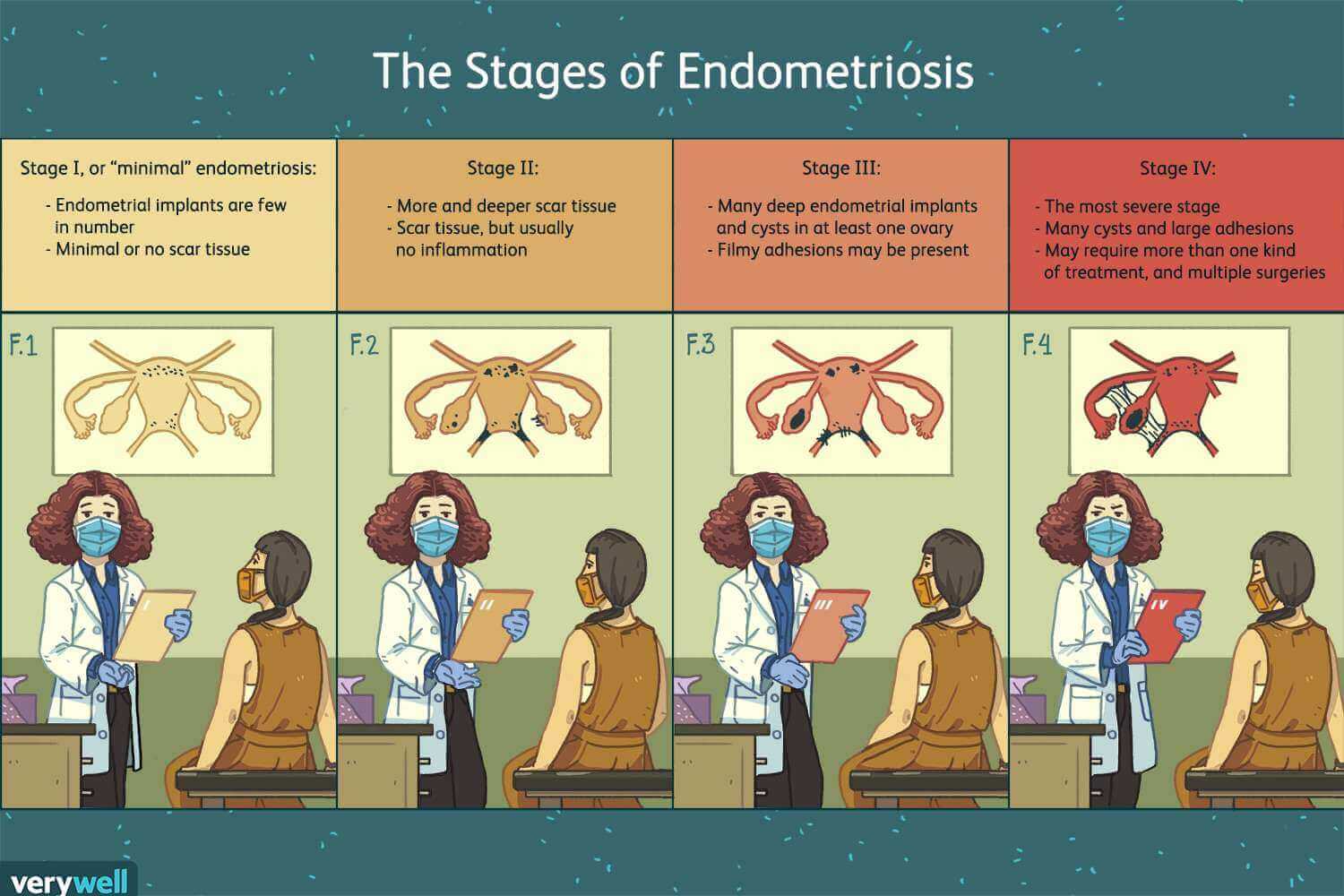
Based on the exact location, the spread of the endometrial tissue, and its depth of infiltration, the scale used to measure endometriosis is that from The American Society of Reproductive Medicine (ASRM).
Results, usually obtained from performing a laparoscopy, are then used to rank the condition. The 4 stages are:
Stage 1 (1-5 points). Minimal. Typically there are only a few small lesions. These lesions may appear on the body’s organs or on the tissue which lines the pelvis or abdomen. During this stage, there is hardly any or even no scar tissue.
Stage 2 (6-15 points). Mild: In the mild stage of endometriosis, there are more lesions when compared to stage 1; located deeper in the tissue. Some scar tissue may be present.
Stage 3 (16-40 points). Moderate: Not only will there be many deep lesions, but small cysts may even be found on one or both of the ovaries, as well as adhesions that are caused by thick bands of scar tissue. Scar tissue forms when the body tries to heal from inflammation caused by endometriosis.
Stage 4 (>40 points). Severe: The most widespread and severe form of endometriosis. There are many deep lesions and thick adhesions throughout the pelvic region. At the least, you will find a large cyst on one or both of the ovaries.
Types of Endometriosis
Since every one of the 4 stages associated with endometriosis has many variations, the Endometriosis Foundation of America (ASRM) proposed using categories that are a whole lot more descriptive.
These different categories are better known as the different types/forms of endometriosis. The 4 principal types are grouped together based on the areas of the abdomen or pelvis that are affected by endometriosis.
- Peritoneal endometriosis. The minimal form of endometriosis. There is a thin membrane, known as the peritoneum, which lines the abdomen and pelvis. Peritoneal endometriosis happens when endometrial tissue attaches to the peritoneum.
- Endometriomas or Ovarian Endometriomas (chocolate cysts). These cysts are dark and fluid-filled, and often referred to as chocolate cysts. They come in different sizes and appear in different parts of the abdomen or pelvis. These cysts, however, mostly appear in the ovaries. A particular concern is that these cysts can break, resulting in endometriosis spreading in the pelvic cavity.
- Deeply infiltrating endometriosis (DIE). The body organs generally affected by this type of endometriosis include the rectum, ovaries, bowels, and bladder. It happens when endometrial tissue invades those organs found either within or outside the pelvic cavity. Although rare (found only between 1 and 5% of women with endometriosis), scar tissue can bond organs so they become stuck in place leading to a condition called “frozen pelvis”.
- Abdominal wall endometriosis. This happens when endometrial tissue grows on the wall of the abdomen. The cells may also attach to a scar from a surgical incision, like for instance, from a C-section.
How is Endometriosis Diagnosed?
The initial questioning of patients by general practitioners, gynecologists, or midwives is able to guide the diagnosis: disabling pain during menstruation, during sexual intercourse, digestive disorders, urinary disorders, uncontrolled bleeding, pain when walking, etc.
Diagnosing endometriosis is a complex matter since the disease takes on different forms. The examinations generally conducted include, but are not limited to:
- Pelvic examination: A physical examination whereby the doctor feels for cysts on the ovaries or scars behind the uterus. Unless areas of endometriosis cause cysts to form, it is very difficult to feel areas of endometriosis. This exam is actually insufficient when it comes to diagnosing endometriosis.
- Ultrasound. Using a device called a transducer, this test uses high-frequency sound waves that create images of the reproductive organs (ovaries, the fallopian tubes, the uterus, the cervix, and the vagina). The transducer can be used in 2 ways; both of which are applied to get the best possible view of the reproductive organs. Either pressed against the abdomen or by insertion into the vagina (known as transvaginal ultrasound). Unfortunately, this test will not confirm the presence of endometriosis, but it does well in identifying endometriomas (cysts that are associated with endometriosis).
- Magnetic resonance imaging (MRI). The MRI test uses radio waves, a magnetic field, and a computer to produce a clear image of the inside of a person’s body (organs and tissue). The MRI can supply detailed information regarding the size and location of endometrial lesions.
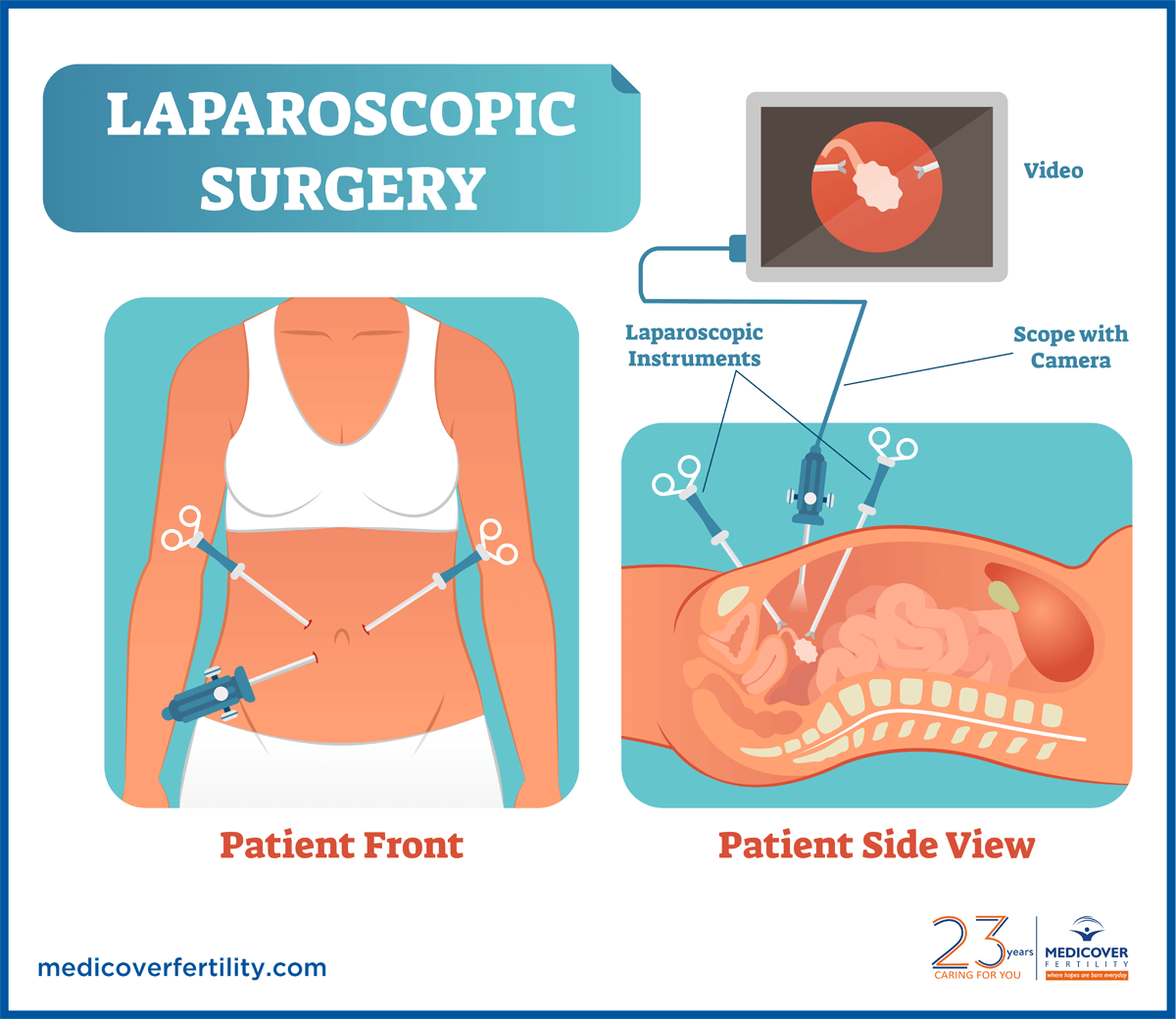
- Laparoscopy. The best way to definitively diagnose endometriosis. In this procedure, a surgeon uses a laparoscope (camera) to view the inside of your abdomen. The procedure is done under general anesthesia. A small cut is made near the navel through which the laparoscope is inserted into the pelvis. The laparoscope is used to look for signs of endometrial tissue outside the uterus. Laparoscopy provides information pertaining to the location, size of the endometrial lesions, and their extent. Endometriosis can at times be confirmed just by seeing the growths. Other times, a sample of the tissue may have to be examined under a microscope to confirm endometriosis.
Endometriosis Treatment
As is the case with chronic diseases, there also is no cure for endometriosis and as a result, it’s important to learn how to manage endometriosis once it has been diagnosed.
The available endometriosis treatment options do help a lot in managing the symptoms associated with the disease.
The best endometriosis treatment is usually done in consultation with the treating doctor. Most doctors will start out endometriosis treatment using conservative methods; recommending other treatments only when these methods fail to bring improvement to the condition.
Endometriosis treatment generally consists of medication or surgery. The severity of a patient’s symptoms as well as the desire to fall pregnant will greatly determine the approach you and your doctor will choose.
Pain medication
The doctor may initially recommend those patients with mild pain symptoms to take over-the-counter pain relievers, such as Advil, and Motrin IB, or Aleve.
Stronger prescription drugs may bring reprieve from very painful menstrual cramps experienced during the menstruation period.
Hormone therapy
When a woman is not trying to fall pregnant, the doctor may prescribe hormone treatment in combination with pain medications. Hormone treatment forms include pills, injections, or nasal spray.
When a patient takes supplemental hormones, the supplements may prove to be quite sufficient in the reduction or even total elimination of the pain associated with endometriosis. Hormonal supplements may also curb the growth of endometriosis.
Using hormone therapy as an endometriosis treatment option stops ovaries from producing hormones such as estrogen, thus preventing ovulation from occurring. This in turn may help slow the progression and local activity of not only the endometrium but also of the endometrial lesions.
This kind of endometriosis treatment (hormone treatment) may slow down the growth of endometrial tissue and also hinder new implants from developing. It will, however, not make existing implants disappear.
Hormone therapies generally suggested to treat endometriosis include:
- Hormonal contraceptives. In endometriosis cases where the disease is of lesser severity, using contraceptives such as patches, vaginal rings, and birth control pills can both reduce and get rid of endometriosis pain.
Many females experience more regular, lighter, and shorter menstruation periods when they use a hormonal contraceptive. Hormonal contraceptives can lessen or even eliminate pain in many instances.
- Gonadotropin-releasing hormone (Gn-RH) drugs send the body into an artificial menopausal state. What this means is these medicines block the production of estrogen resulting in lower estrogen levels and thus prevents menstruation. This in turn causes the endometrial tissue to shrink.
In order to limit the typical menopausal side effects, such as vaginal dryness, hot flashes, and bone loss, it is recommended to take a small dose of progestin or estrogen along with Gn-RH agonists and antagonists. Normal menstrual periods as well as the ability to fall pregnant return when these drugs are no longer taken.
GnRH drugs are available in injections and nasal sprays forms.
- Progestin and progesterone therapy. For women who cannot take estrogen because of risks such as cardiovascular disease or blood clots, progestin-only drugs are prescribed. These drugs reduce the menstrual flow.
Progestin contraceptive therapy is available in pill (Camila), injection (Depo-Provera), an implant (Nexplanon), and an intrauterine device (IUD) with levonorgestrel (Mirena, Skyla) forms.
Endometriosis symptoms are improved when these hormonal contraceptives halt the menstrual period and stop the progression of endometrial lesions. Falling pregnant is also prevented.
- Aromatase inhibitors. A class of medicines that lower the measure of estrogen in your body.
A progestin or combination of hormonal contraceptives may be prescribed by the treating doctor as an endometriosis treatment option.
A permanent solution?
Hormone therapy, unfortunately, is not necessarily the best endometriosis treatment option or even a permanent fix.
Relief from the pain usually associated with endometriosis lasts only as long as the symptoms are treated. Once endometriosis treatment stops, endometriosis symptoms may reoccur, and the ability to fall pregnant returns.
A lot of women choose to carry on with endometriosis treatment indefinitely. Some women are lucky enough to not experience pain for a number of years after they stopped treatment.
Surgical endometriosis treatment options
Surgery is an endometriosis treatment option usually pursued when pain and hormonal treatments do not work. While surgical treatments do provide great relief from the pain associated with endometriosis, relief is short-term only.
If someone suffers from endometriosis but also wants to fall pregnant, the surgery options available must be well understood and discussed with the surgeon before deciding which procedure to undergo. Not all procedures can be reversed and may affect the ability to fall pregnant.
Surgical procedures generally are done not only to get rid of endometriosis implants but at the same time to preserve the reproductive organs.
When the pain from endometriosis is severe, the sufferer may also benefit from surgery. There is, however, no guarantee that this is the ultimate cure for either endometriosis or pain.
Laparoscopy
In the surgical process, known as laparoscopy, even cases where the condition of endometriosis is considered severe can be treated.
In laparoscopic surgery, the surgeon first uses an instrument and gas to inflate the abdomen. A laparoscope (a viewing instrument that comes with a light), is inserted through a small cut close to the navel in order to view the endometrial growths.
In order to either remove or destroy the endometriosis implants, the surgeon uses other surgical instruments or lasers.
In a process called excising, endometrial tissue is removed through another small cut in the abdomen.
When endometrial implants need to be destroyed, a process known as cauterization is used. Destruction happens with the application of intense heat from a laser and the blood vessels are sealed without the need for stitches.
After surgery, the surgeon may recommend hormonal drugs to bring relief from the pain.
“With surgery, most women have pain relief in the short term, but pain often returns. Surgery can provide long-term pain relief in women with deep lesions when those lesions are excised.” Source
Hysterectomy
There was a time when a total hysterectomy was thought of as the best and most effective endometriosis treatment option. With a total hysterectomy, both the uterus (hysterectomy) and the ovaries (oophorectomy) are removed.
Not anymore. Nowadays, doctors rarely recommend a hysterectomy to get rid of endometriosis, except in instances where the symptoms remain severe despite different endometriosis treatments, and the woman affected does not wish to fall pregnant later on.
Experts now rather focus on removing all endometrial tissue in a thorough and careful manner.
When ovaries are removed, menopause starts. Since there are no longer ovaries that produce hormones, the pain associated with endometriosis may improve for some women. For others, however, should any endometrial tissue remain after surgery, symptoms may still be experienced.
There are risks associated with early menopause, a number of metabolic conditions (dyslipidemia, impaired glucose tolerance, insulin resistance, hyperinsulinemia, and type 2 diabetes), cardiovascular diseases, and premature death.
When the surgeon recommends the removal of the uterus it is to bring relief from endometriosis symptoms such as uterine cramps and heavy menstrual bleeding. It is only recommended for women who do not wish to fall pregnant at a later stage.
For women who decide to have a hysterectomy (removal of the uterus) at an age younger than 35 years, the surgery may affect their health long-term, even if the ovaries are not removed.
It is vital to find a doctor to help you manage and treat endometriosis with whom you are comfortable. It may be advantageous to look for a second opinion before embarking on any endometriosis treatment.
Women need to familiarize themselves with and understand all the endometriosis treatment options available. They also need to be advised on the possible outcomes to expect from each endometriosis treatment option.
Conclusion
Endometriosis is a chronic condition that causes no symptoms at all in some women, while other women suffer from it a lot in their everyday lives.
Treatment reduces the symptoms, but they usually do not disappear completely. Endometriosis is not life-threatening. When mild endometriosis is experienced, treatment is often not necessary. In more severe forms treatment may be necessary.
As mentioned, discuss with your gynecologist which treatments are possible for your specific condition. Your gynecologist will indicate whether you can wait and see how the endometriosis develops, or whether it is wise to start treatment and which endometriosis treatment option is best.