To meaningfully discuss the different types of autoimmune diseases, we first need to understand what autoimmune diseases are and how they are classified.
Page Contents
What are Autoimmune Diseases?
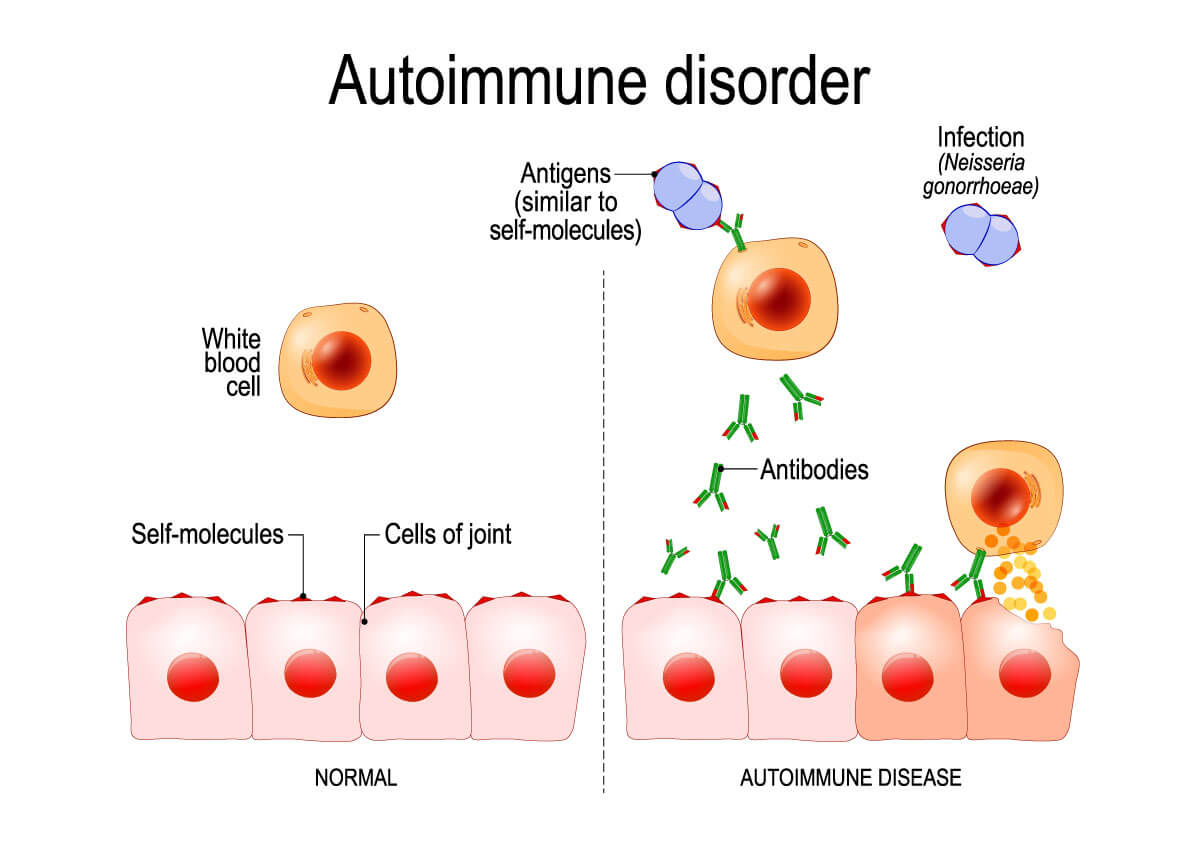
When you are healthy, your body’s immune system can tell the difference between your body’s healthy cells and foreign cells.
In an autoimmune disease, however, the body mistakes its own cells as foreign. In response, proteins that are called autoantibodies are released which attack healthy cells.
A healthy immune system works actively against diseases and as such fends off invaders.
When your body’s own immune system turns against your body, you develop an autoimmune disease that can either affect the whole body or attacks specific organs in the body.
There are many diseases of which it is now known are caused by autoimmunity.
Who gets affected by autoimmune diseases?
Autoimmune diseases occur mainly in adults and less often in children and the elderly.
More women than men are affected. Autoimmune diseases often start in women during childbearing age.
People with autoimmune diseases running in the family have an increased risk.
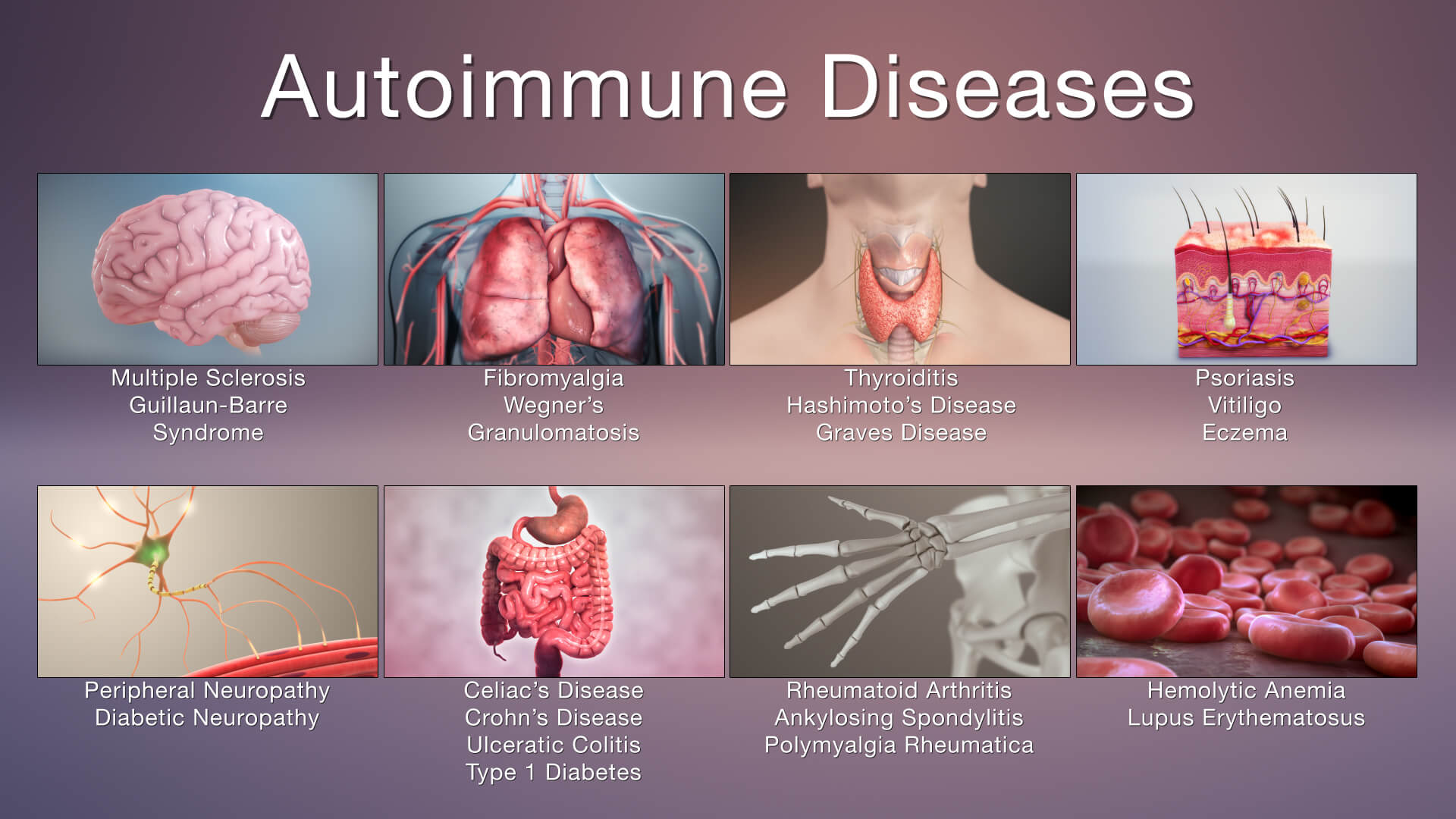
Image source
What are the Causes of Autoimmune Diseases?
The cause is still unknown with researchers still trying to ascertain what exactly the causes of autoimmune diseases are.
Autoimmune diseases are more common in some families, so hereditary factors play a role.
There are also certain factors that can trigger an autoimmune response. Think of viral and bacterial infections or an adverse reaction to certain medicines.
Race and ethnic background play a role in the severity of autoimmune diseases in people. Lupus is more severe in African-American people. Type 1 diabetes is more commonly found in white people.
One person can have multiple autoimmune diseases.
Autoimmune diseases are probably caused by a combination of hereditary predisposition and environmental factors such as infections.
Exposure to sunlight and certain solvents may also be a contributing factor to consider as to why some people develop an autoimmune disease.
Autoimmune diseases are more common in women than in men, as hormonal influences may play a role.
Science has been investigating the exact causes of autoimmune diseases for many years.
Is the cause primarily physical or are there perhaps more psychological or environmental factors that need to be considered?
What is certain for the time being is that there is a genetic component. It must be a natural predisposition. However, the predisposition is not certain to develop. It may happen to one individual, but not necessarily to another.
Environmental factors and more psychological characteristics may or may not cause autoimmune diseases to actually manifest themselves.
Aging, stress, infections, and hormonal changes are examples of influences that partly determine whether you will develop an autoimmune disease or not, even if you have a genetic predisposition.
Another risk factor considered by scientists is a diet that consists of high-sugar, high-fat, and processed foods.
How common are these diseases?
Some of these diseases (such as rheumatism, Crohn’s disease, or Multiple Sclerosis) are more common than others (Sjogren’s, Addison’s disease, or Lupus).
Autoimmune diseases are more common in women and especially in women of childbearing age. Geography and origin also seem to play a role, but the research results are not unequivocal about this.
Autoimmune diseases are relatively more common in the United States and other Western countries.
What Are The Common Symptoms Of Autoimmune Diseases?
At the time of writing, there are more than 100 autoimmune diseases in existence. The severity of these ranges from very mild to disabling, depending on which part or organ of the body is under attack.
The symptoms will therefore differ depending on the specific disease. Also, symptoms may be mild in some people while in others it could be so severe it leads to hospitalization.
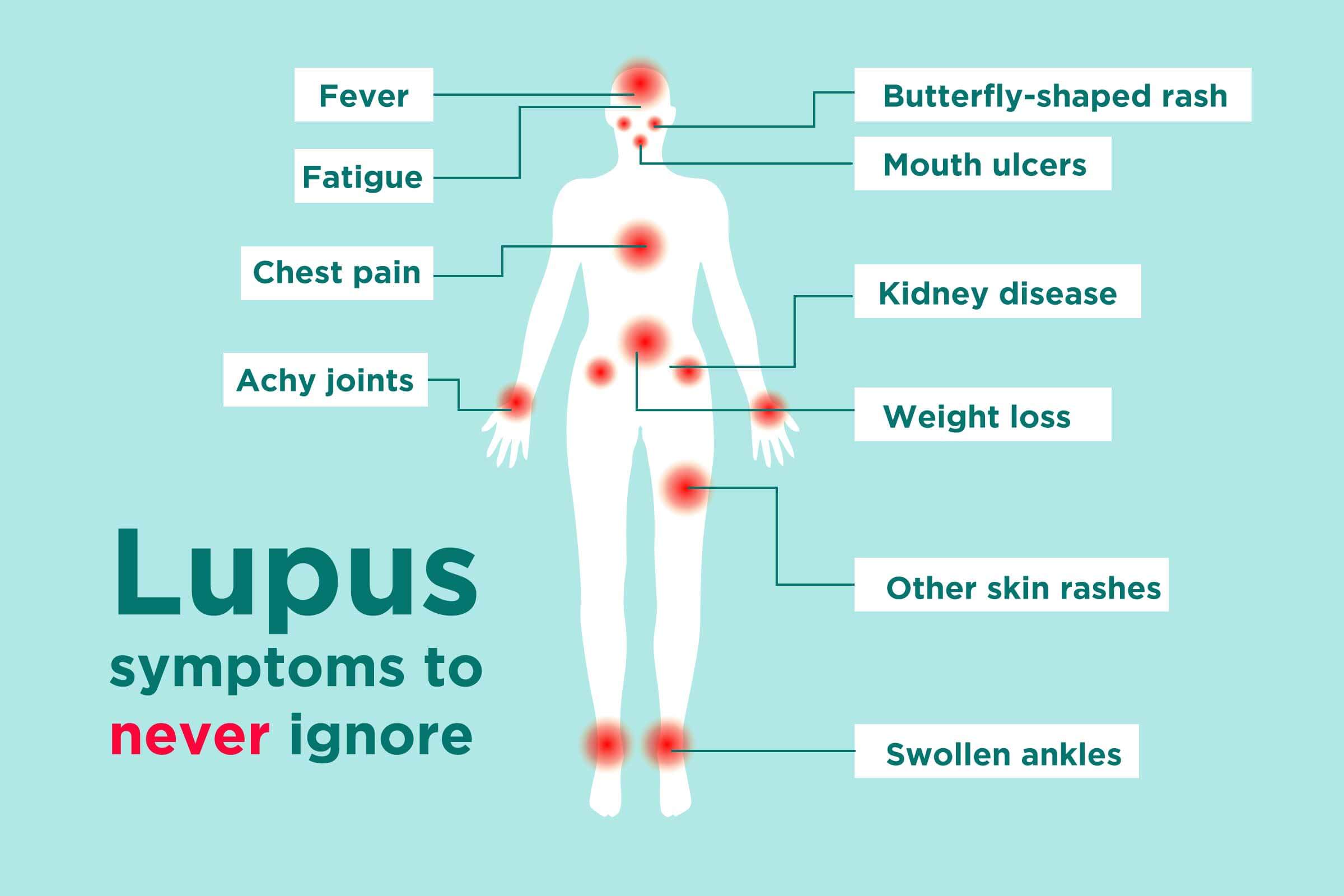
In general, however, even though there are so many different autoimmune diseases, some of them share similar symptoms.
Some of the symptoms that are similar in some types of autoimmune diseases are:
- Fatigue or chronic tiredness. The loss of energy is caused by the immune system using the body’s energy to fight “invaders”.
- Recurring fever
- Swollen glands. Autoimmune diseases that can cause swollen glands are rheumatoid arthritis and systemic lupus erythematosus.
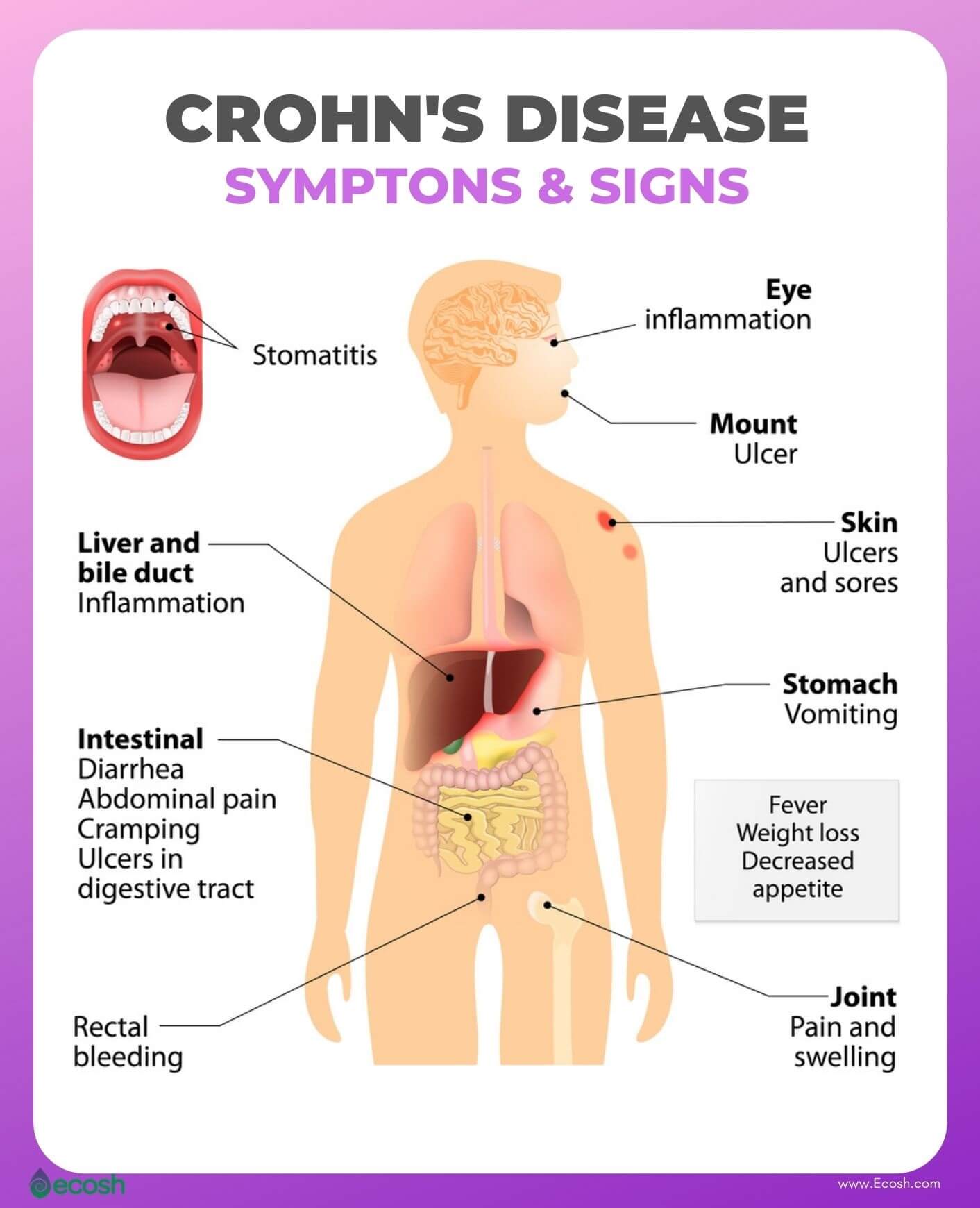
- Pain in the abdomen and digestive problems. Crohn’s disease and ulcerative colitis affect the bowels. These inflammatory bowel diseases can add to the discomfort experienced.
- Skin rashes and/or lesions. Typical of psoriasis. Skin cells multiply so fast it forms dry and scaly patches which itch.
- Pain and swelling in the muscles, joints, and/or connective tissues. It happens when the body’s immune system attacks healthy muscle tissue. Muscle weakness is the result of inflammation, swelling, and pain.
- Lack of concentration (brain fog). Frequently experienced by people who suffer from fibromyalgia (70-80%) or systemic lupus erythematosus 30-40%). Other characteristics include lack of focus and mental clarity. Increased forgetfulness and fatigue. Low energy levels.
- Numbness and tingling in arms and legs. Especially a sign that MS (multiple sclerosis) is developing.
- Autoimmune inner ear disease (AIED) is a rare disease and the result of your immune system attacking the inner ear. Can also cause ringing in the ears and hearing loss.
- Weight gain. May be an indication that the thyroid glands do not produce the hormones needed to function properly. This may result in the autoimmune disease known as Hashimoto’s thyroiditis.
The classic symptom of most types of autoimmune diseases is inflammation. The inflammation may cause redness, pain, heat, and swelling.
Autoimmune diseases are generally characterized by alternating episodes in which symptoms occur and in which a patient is relatively symptom-free.
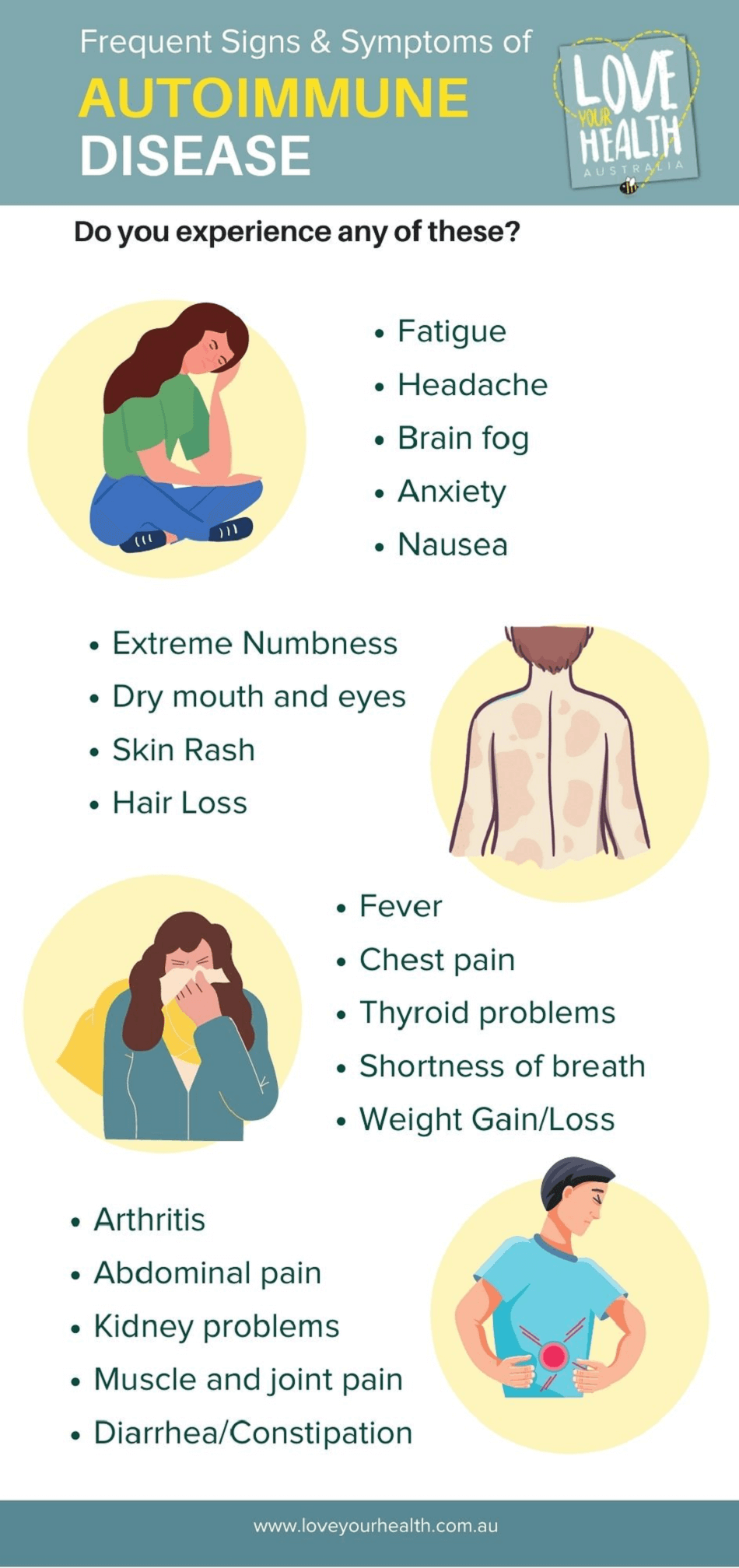
Image courtesy loveyourhealth
What Are The Different Types Of Autoimmune Diseases?
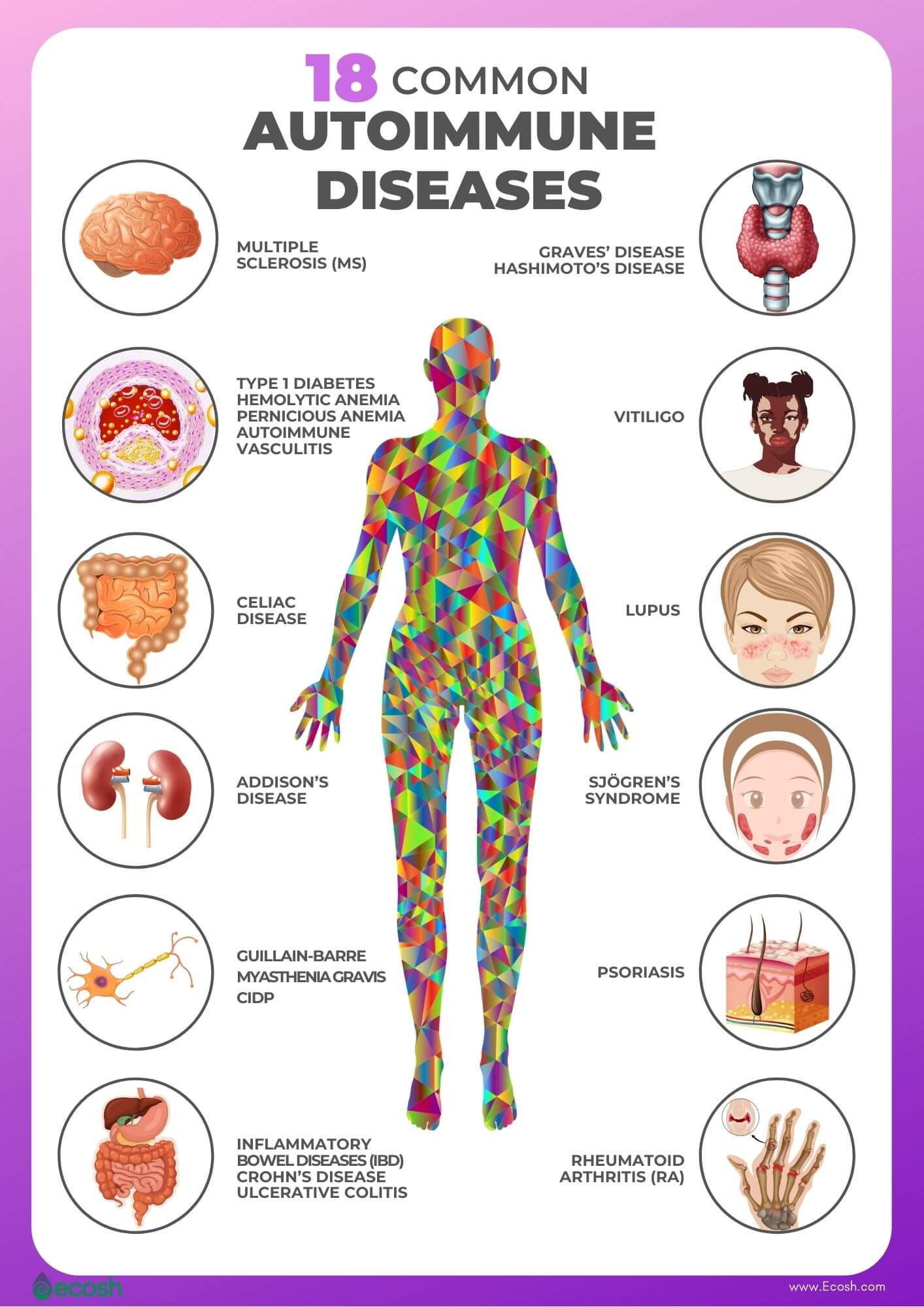
Autoimmune diseases belong to one of the two classes identified as follows:
SYSTEMIC DISORDERS
Systemic disorders are one of the types of autoimmune diseases that affect many different organs and tissue of the human body.
These disorders are characterized by dysregulation of the immune system which gives rise to activation of immune cells to attack autoantigens and result in inappropriate inflammation and multi-tissue damages. Source.
Examples of systemic autoimmune diseases include rheumatoid arthritis (RA), Sjogren’s syndrome, systemic lupus erythematosus (SLE), dermatomyositis, and scleroderma.
ORGAN-SPECIFIC DISORDERS
Organ-specific (local) types of autoimmune diseases happen when the body’s immune system attacks a particular organ or tissue.
Organ-specific diseases commonly known include Type 1 diabetes mellitus, Graves’ disease, Hashimoto’s thyroiditis, Addison’s disease, Autoimmune hepatitis, Celiac disease, gastritis, vitiligo, hepatitis, Myasthenia Gravis, psoriasis, multiple sclerosis (MS), etc.
Organ-specific disorders are further divided into different types of autoimmune diseases and refer to a specific organ or tissue:
- Dermatologic diseases include a variety of skin rashes and infections, such as psoriasis, vitiligo, vasculitis, etc.
- Endocrinologic diseases relate to the endocrine glands of the body. The endocrine system produces hormones. Graves’ disease, Addison’s disease, type 1 diabetes mellitus, and Hashimoto’s thyroiditis are examples.
- Neurologic diseases are disorders that affect the brain as well as the nerves found throughout the human body and the spinal cord. Guillain-Barré syndrome, MS (multiple sclerosis), and myasthenia gravis are examples of the immune system attacking healthy nerve cells.
- Hematologic diseases are disorders of the blood and blood-forming organs. Examples are Hemolytic anemia, antiphospholipid syndrome, thrombotic thrombocytopenic purpura, Evans syndrome, and autoimmune neutropenia.
- Gastrointestinal (GI) diseases affect any section of the gastrointestinal tract, from the esophagus to the rectum, and the accessory digestive organs such as the liver, gall bladder, and pancreas. Gastrointestinal disorders include Inflammatory Bowel Disease (IBD) in the form of Crohn’s disease and Ulcerative Colitis. Celiac disease is another common disorder that affects the gastrointestinal tract.
A list of autoimmune diseases:
- Achalasia
- Addison’s disease
- Adult Still’s disease
- Agammaglobulinemia
- Alopecia areata
- Amyloidosis
- Ankylosing spondylitis
- Anti-GBM/Anti-TBM nephritis
- Antiphospholipid syndrome
- Autoimmune angioedema
- Autoimmune dysautonomia
- Autoimmune encephalomyelitis
- Autoimmune hepatitis
- Autoimmune inner ear disease (AIED)
- Autoimmune myocarditis
- Autoimmune oophoritis
- Autoimmune orchitis
- Autoimmune pancreatitis
- Autoimmune retinopathy
- Autoimmune urticaria
- Axonal & neuronal neuropathy (AMAN)
- Baló disease
- Behcet’s disease
- Benign mucosal pemphigoid
- Bullous pemphigoid
- Castleman disease (CD)
- Celiac disease
- Chagas disease
- Chronic inflammatory demyelinating polyneuropathy (CIDP)
- Chronic recurrent multifocal osteomyelitis (CRMO)
- Churg-Strauss Syndrome (CSS) or Eosinophilic Granulomatosis (EGPA)
- Cicatricial pemphigoid
- Cogan’s syndrome
- Cold agglutinin disease
- Congenital heart block
- Coxsackie myocarditis
- CREST syndrome
- Crohn’s disease
- Dermatitis herpetiformis
- Dermatomyositis
- Devic’s disease (neuromyelitis optica)
- Discoid lupus
- Dressler’s syndrome
- Endometriosis
- Eosinophilic esophagitis (EoE)
- Eosinophilic fasciitis
- Erythema nodosum
- Essential mixed cryoglobulinemia
- Evans syndrome
- Fibromyalgia
- Fibrosing alveolitis
- Giant cell arteritis (temporal arteritis)
- Giant cell myocarditis
- Glomerulonephritis
- Goodpasture’s syndrome
- Granulomatosis with Polyangiitis
- Graves’ disease
- Guillain-Barre syndrome
- Hashimoto’s thyroiditis
- Hemolytic anemia
- Henoch-Schonlein purpura (HSP)
- Herpes gestationis or pemphigoid gestationis (PG)
- Hidradenitis Suppurativa (HS) (Acne Inversa)
- Hypogammalglobulinemia
- IgA Nephropathy
- IgG4-related sclerosing disease
- Immune thrombocytopenic purpura (ITP)
- Inclusion body myositis (IBM)
- Interstitial cystitis (IC)
- Juvenile arthritis
- Juvenile diabetes (Type 1 diabetes)
- Juvenile myositis (JM)
- Kawasaki disease
- Lambert-Eaton syndrome
- Leukocytoclastic vasculitis
- Lichen planus
- Lichen sclerosus
- Ligneous conjunctivitis
- Linear IgA disease (LAD)
- Lupus
- Lyme disease chronic
- Meniere’s disease
- Microscopic polyangiitis (MPA)
- Mixed connective tissue disease (MCTD)
- Mooren’s ulcer
- Mucha-Habermann disease
- Multifocal Motor Neuropathy (MMN) or MMNCB
- Multiple sclerosis
- Myasthenia gravis
- Myelin Oligodendrocyte Glycoprotein Antibody Disorder
- Myositis
- Narcolepsy
- Neonatal Lupus
- Neuromyelitis optica
- Neutropenia
- Ocular cicatricial pemphigoid
- Optic neuritis
- Palindromic rheumatism (PR)
- PANDAS
- Paraneoplastic cerebellar degeneration (PCD)
- Paroxysmal nocturnal hemoglobinuria (PNH)
- Parry Romberg syndrome
- Pars planitis (peripheral uveitis)
- Parsonage-Turner syndrome
- Pemphigus
- Peripheral neuropathy
- Perivenous encephalomyelitis
- Pernicious anemia (PA)
- POEMS syndrome
- Polyarteritis nodosa
- Polyglandular syndromes type I, II, III
- Polymyalgia rheumatica
- Polymyositis
- Postmyocardial infarction syndrome
- Postpericardiotomy syndrome
- Primary Biliary Cholangitis
- Primary sclerosing cholangitis
- Progesterone dermatitis
- Psoriasis
- Psoriatic arthritis
- Pure red cell aplasia (PRCA)
- Pyoderma gangrenosum
- Raynaud’s phenomenon
- Reactive Arthritis
- Reflex sympathetic dystrophy
- Relapsing polychondritis
- Restless legs syndrome (RLS)
- Retroperitoneal fibrosis
- Rheumatic fever
- Rheumatoid arthritis
- Sarcoidosis
- Schmidt syndrome
- Scleritis
- Scleroderma
- Sjögren’s syndrome
- Sperm & testicular autoimmunity
- Stiff person syndrome (SPS)
- Subacute bacterial endocarditis (SBE)
- Susac’s syndrome
- Sympathetic ophthalmia (SO)
- Takayasu’s arteritis
- Temporal arteritis/Giant cell arteritis
- Thrombocytopenic purpura (TTP)
- Thyroid eye disease (TED)
- Tolosa-Hunt syndrome (THS)
- Transverse myelitis
- Type 1 diabetes
- Ulcerative colitis (UC)
- Undifferentiated connective tissue disease (UCTD)
- Uveitis
- Vasculitis
- Vitiligo
- Vogt-Koyanagi-Harada Disease
The source of the above list is AARDA.
Diagnosing Autoimmune Diseases
It is difficult to diagnose almost all types of autoimmune diseases and there is no single method only used to diagnose any suspected autoimmune disease.
An accurate diagnosis can never be made on the basis of symptoms such as fatigue and recurrent inflammation alone.
The physician may enquire about your medical history during diagnosis.
Generally, the medical practitioner uses a combination of other tests and a physical examination to assist in determining the exact autoimmune disease.
- The most common blood test is the ANA (antinuclear antibody test) which is used to detect autoantibodies. Is initially used when an autoimmune disease, based on symptoms, is suspected. While it may produce a positive test, it is not able to confirm which autoimmune disease a person has.
- Other blood tests used for diagnosis are 1) the (preferred) test known as C-reactive protein (CRP) and 2) erythrocyte sedimentation rate (ESR). These tests are used to assess inflammation not caused by an infection or the result of other reasons.
- Tissue and muscle biopsies make it easier to diagnose autoimmune diseases like lupus and myositis.
- X-rays are used to look at joints in the body.
Autoimmune Diseases Treatment
Autoimmune diseases are largely incurable, but there are treatments that can control many of the conditions.
As mentioned earlier, a critical symptom of autoimmune diseases is inflammation and this subsequently is also the main reason for not feeling well.
To combat the diseases, anti-inflammatories and immune-suppressing drugs are prescribed.
In aggressive forms of autoimmune diseases, suppressing the immune system is the most important.
When you, however, suppress the functioning of the immune system, the body is also less able to fight off real invaders. There is therefore a greater risk of bacterial and viral infections.
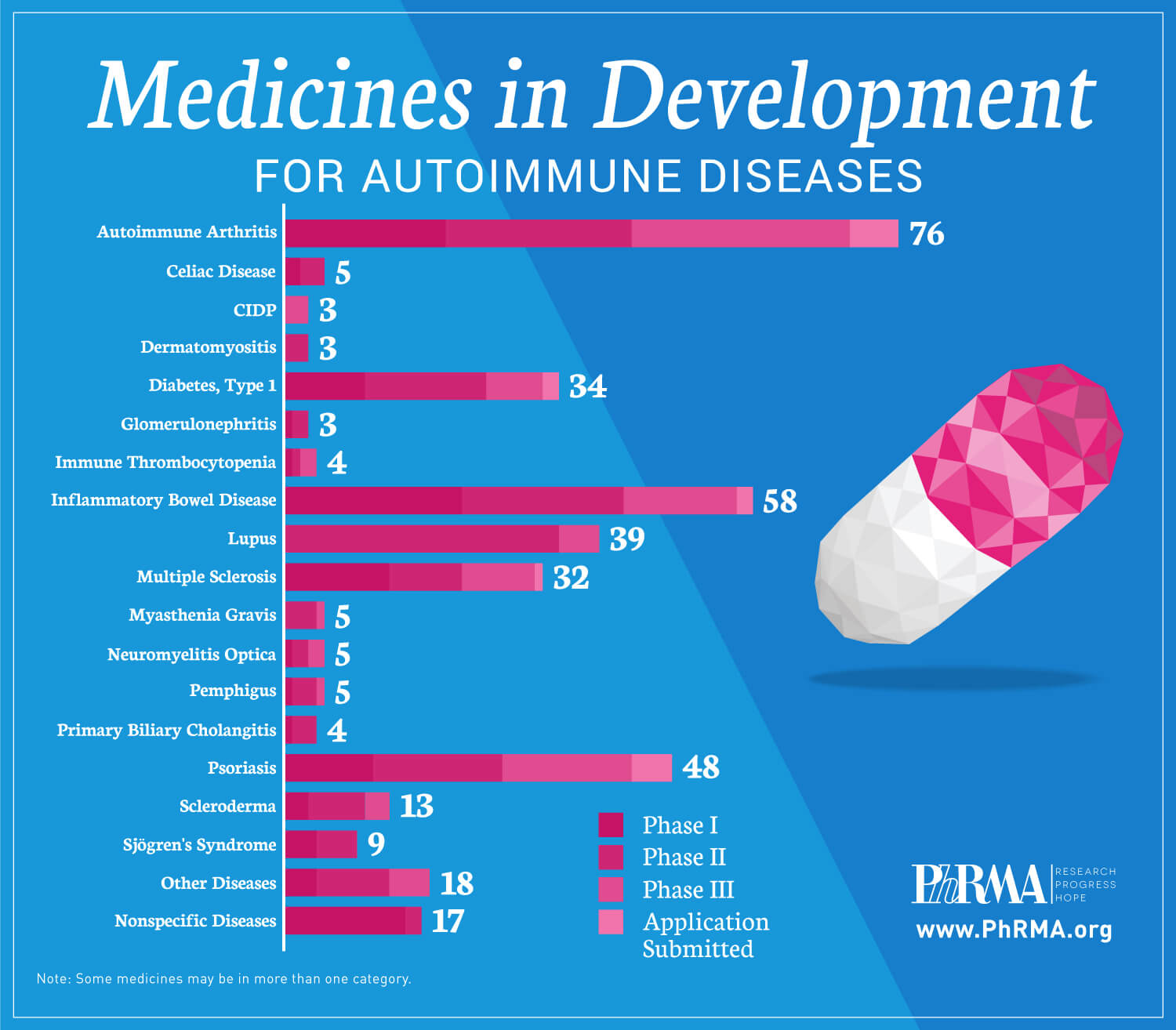
Image courtesy statnews
Treatments that are generally prescribed for autoimmune diseases are:
- Anti-inflammatory drugs – to reduce inflammation and pain
- Corticosteroids – to reduce inflammation. They are sometimes used to treat an acute flare of symptoms
- Pain killers – such as paracetamol and codeine
- Immunosuppressant drugs – to inhibit the activity of the immune system. The use of immune system suppressing drugs has been tried recently, with promising results. Particularly when intervention is early, the chance of a cure with some of these conditions seems possible.
- Physical therapy – to encourage mobility
- Treatment for the deficiency – for example, insulin injections in the case of diabetes
- Surgery – for example, to treat bowel blockage in the case of Crohn’s disease
In general, it is quite possible to live with autoimmune diseases treated with medication.
On the whole, those affected by any one of the autoimmune diseases experienced them as very difficult.
With most autoimmune diseases, you can grow old. You will, however, live a life in which you often feel very ill and be unable to do as much as other people.