What is fibromyalgia?
Fibromyalgia (fiber muscle pain) is a chronic pain disorder that is sometimes referred to as fibromyalgia syndrome (FMS).
Deep muscle and joint pain in the right and left sides of the upper and lower body is how the condition is best described. The condition may be accompanied by issues relating to insomnia, fatigue, concentration problems, exhaustion, and mood swings.
Many people who suffer from fibromyalgia also experience depression, anxiety, migraines, TMJ (temporomandibular joint) disorders, interstitial cystitis (painful bladder syndrome), postural orthostatic tachycardia syndrome (POTS), and disturbed bowel functions (IBS).
A lot more females than males are affected by fibromyalgia. In the US, about 2% of the adult population suffers from fibromyalgia and the age of onset is generally at 35.
Organs, muscles, ligaments, or tendons are not damaged by fibromyalgia.
What Causes Fibromyalgia?
Fibromyalgia causes are largely still unknown. Triggers regarded as a root cause for fibromyalgia seem to be either a physical or emotionally stressful event.
A genetic predisposition is also suspected to be a trigger for fibromyalgia to flare up.
Fibromyalgia syndrome is not a rheumatic disease, nor is it inflammation or a disease caused by wear and tear.
According to the current state of knowledge, the central nervous pain perception is changed in those affected. Due to a lower level of perception of pain, the brain assigns disproportionately greater importance to even slight pain. The increased pain sensitivity could also be inherited. This is supported by the fact that relatives have an increased risk of being affected by fibromyalgia.
For a long time, fibromyalgia sufferers were viewed as hypochondriacs because there was no evidence of their pain. Today this has been refuted, even if psychological factors play an essential role in the development of pain. Because stress, whether in a positive or negative form, can aggravate pain.
It is known that people who have experienced severe trauma in childhood or as adults are more likely to suffer from fibromyalgia. Fibromyalgia has been associated with PTSD (post-traumatic stress disorder).
Fibromyalgia can also develop when people have other medical conditions. One then speaks of secondary fibromyalgia. The following diseases favor the outbreak: rheumatism, infectious diseases (mostly viral infections with the Epstein-Barr virus, hepatitis viruses, and HI viruses), some tumor diseases, and hormonal disorders.
Signs of Fibromyalgia
Anyone suffering from fibromyalgia suffers from chronic pain and muscle tension all over the body.
Often there are also emotional complaints. The pain is usually focused on certain parts of the body and has existed for at least three months. The neck, back, arms, legs, and chest are often affected.
Those affected often react very sensitively to stimuli such as smells, cold, noise, and bright light. Fibromyalgia patients are more sensitive to pain.
A distinction is made between core symptoms, such as chronic muscle and limb pain, fatigue, difficulty falling asleep and staying asleep, and feelings of swelling, from other accompanying symptoms.
Patients with these additional symptoms have a severe form of fibromyalgia syndrome. The intensity of the complaints is not the same every day. Pain-free times are also possible.
Signs of fibromyalgia include:
- Joint and muscle pain
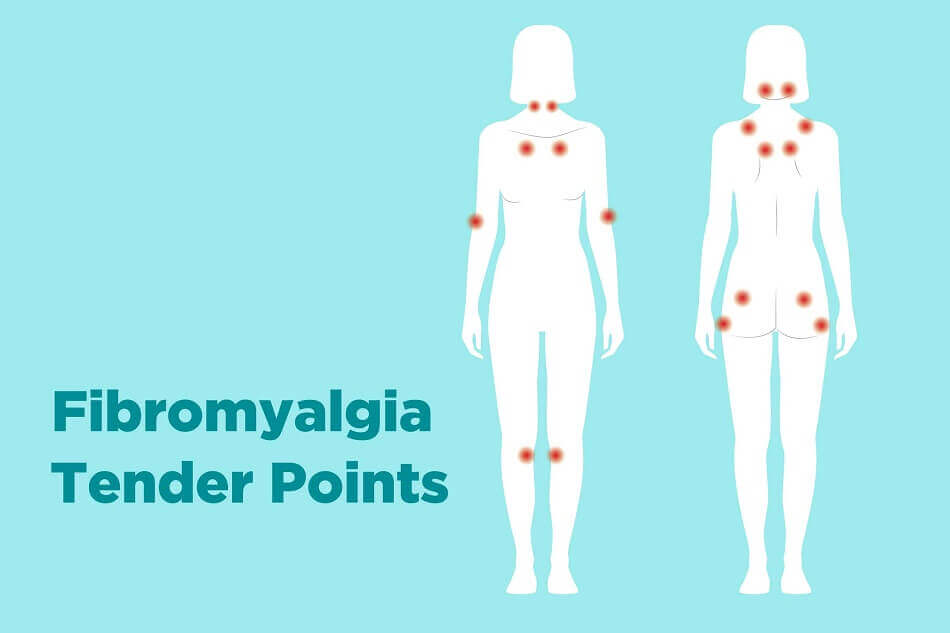
- Painful pressure points (so-called tender points)
- Pain in the tendons
- Stiffness
- Headaches and migraine
- Irritable bowel syndrome, often associated with abdominal pain, constipation, or diarrhea
- Irritable bladder (constant need to urinate)
- Difficulty sleeping (difficulty falling or staying asleep)
- Fatigue is more often than not caused by disruption of sleep due to pain, and not due to lack of adequate sleeping time. Sleep disorders such as sleep apnea and restless leg syndrome that many fibromyalgia patients suffer from, also play a role.
- Difficulty concentrating, memory lapses, and difficulty staying alert. These signs of fibromyalgia are commonly known as “fibro fog” or “brain fog”. Fibro fog may also result in a patient’s inability to hold a conversation or access information stored in the brain quickly enough. Many patients find fibro fog a lot more disturbing than the pain normally associated with fibromyalgia.
- Feelings of numbness or swelling in the hands and feet.
- Sensitive mucous membranes associated with a burning sensation
- Hyperalgesia: increased sensitivity to feeling pain and extreme response to pain – Source
- Very low pain threshold: stimuli that others do not perceive as painful are perceived as painful. Something elementary as combing hair or wearing a cotton shirt may cause the fibromyalgia sufferer severe pain. This kind of extreme sensitivity to touch is known as allodynia (type of neuropathic pain).
- Depression is one of the common signs of fibromyalgia. Some researchers study the effects of depression on brain chemistry. Others look at abnormalities of the sympathetic nervous system — the part of the nervous system that determines how you handle stress and emergencies. These abnormalities, they contend, may lead to the release of substances that cause more sensitivity to pain. The result is fibromyalgia with its chronic pain and feelings of depression – Source
- Anxiety disorders are thought of as secondary symptoms associated with fibromyalgia. Between 13% and 71% of patients are affected.
Fibromyalgia Diagnosis
Very often, it takes a very long time before patients are diagnosed with fibromyalgia as there are no specific tests that can be used to diagnose fibromyalgia.
Because of the variety of symptoms associated with fibromyalgia, it is a whole lot more difficult to identify the disease, compared to others.
There are no physical signs on the body, blood tests and x-rays also cannot provide any valuable information. These tests do, however, assist when they are used to rule out other diseases.
Diseases that present much of the same symptoms as fibromyalgia include
- inflammatory and rheumatic diseases such as rheumatoid arthritis, lupus, and Sjogren’s syndrome
- depression and anxiety: these mental disorders often also feature aches and pain
- neurological disorders such as MS (multiple sclerosis) and myasthenia gravis (a neuromuscular disease, causing weakness in the body’s skeletal muscles). Symptoms that feature in these disorders are numbness and tingling.
How is fibromyalgia diagnosed?
The first point of contact is usually the family doctor who will inquire about the patient’s medical and family history. The doctor may also conduct both a physical examination of the patient’s joints and muscles as well as a neurological exam. The doctor will also inquire about how symptoms affect the patient’s daily activities.
The main characteristic of fibromyalgia is widespread pain throughout the patient’s body and should’ve been experienced for a minimum of 3 months. Pain should also have occurred in 4 out of the 5 areas generally associated with fibromyalgia pain.
The 5 areas of the body commonly affected by fibromyalgia pain are:
- Right and left upper regions (jaw, shoulder, arm)
- Right and left lower regions (leg, hip, buttocks)
- Axial area: abdomen, neck, back, and chest regions
Blood tests that the doctor may perform to eliminate other conditions are:
A full blood count: these tests are performed to evaluate the patient’s overall health condition and also to detect the prevalence of any other disease or condition, i.e. anemia, infection, or leukemia.
Erythrocyte sedimentation rate (ESR): done to reveal any inflammatory activity in a patient’s body.
Cyclic citrullinated peptide test (CCP): used to detect and measure the CCP antibodies in the patient’s blood.
Rheumatoid factor (RF): An autoantibody that is produced by the body’s immune system. RF autoantibodies erroneously attack healthy cells and body tissue.
Thyroid function tests: are performed to measure how well the patient’s thyroid gland functions. The different tests are known as T3, T3RU, T4, AND TSH.
Anti-nuclear antibody (ANA): is performed to detect, measure, and evaluate antinuclear antibodies in the patient’s blood. The presence of antinuclear antibodies may indicate an autoimmune disease.
Celiac serology: is a simple blood test that helps in diagnosing celiac disease which is associated with a variety of autoantibodies found in the blood.
Vitamin D: test measures how much vitamin D is in the patient’s body. Vitamin D is an essential nutrient needed for proper growth and the formation of teeth. Medical conditions that can arise from abnormal levels include nutrition problems, bone disorders, or organ damage.
When a patient experiences a sleep disorder, like sleep apnea, an overnight sleep study may be recommended by the treating physician.
Quite often, patients may have another health issue that can coexist with fibromyalgia. The doctor may subsequently inquire if the patient also experiences any of these conditions. Typically the conditions include but are not limited to IBS (irritable bowel syndrome), TMJ (temporomandibular joint syndrome), headaches (especially migraines), painful and frequent urination, depression, anxiety, etc.
A fibromyalgia tender points (aka fibromyalgia pressure points or fibromyalgia trigger points) examination used to be the official diagnostic criterium applied to diagnose fibromyalgia. The tender/pressure points are 18 areas on the patient’s body. The doctor may still use this to check for the pressure points generally associated with fibromyalgia. Using the tip of his/her finger, the doctor will apply pressure on the areas of the tender points to determine if the patient feels any pain.
Fibromyalgia pain points are illustrated in the image below:
Fibromyalgia Treatment
At this time, there is no cure for fibromyalgia.
As is the case with so many other diseases for which there is no cure, fibromyalgia treatment’s main focus is also the reduction of the disease’s symptoms to enhance the sufferer’s quality of life.
It is worth noting that fibromyalgia has no damaging effects on organs, muscles, ligaments, or tendons. It is therefore important for those affected to learn to live with the disease.
Depending on the severity of fibromyalgia, doctors and therapists recommend multimodal therapy with different components. Since the severity of the symptoms varies from patient to patient, it is not possible to give general tips for therapy. Each fibromyalgia disease is individual and should be treated in the same way. Patients are therefore advised to pay close attention to what is personally good for them and what is not.