The symptoms of achalasia usually start out in a gradual manner but get worse as time goes by. Learn more about what causes achalasia symptoms and the most current methods used to treat achalasia.
Page Contents
Achalasia Definition
What is achalasia? The Oxford Languages defines achalasia as follows: “a condition in which the muscles of the lower part of the esophagus fail to relax, preventing food from passing into the stomach.”
Achalasia is a rare chronic disease of the esophagus.
Achalasia may also be called by other names such as achalasia cardiae, cardiospasm, esophageal achalasia, and esophageal aperistalsis.
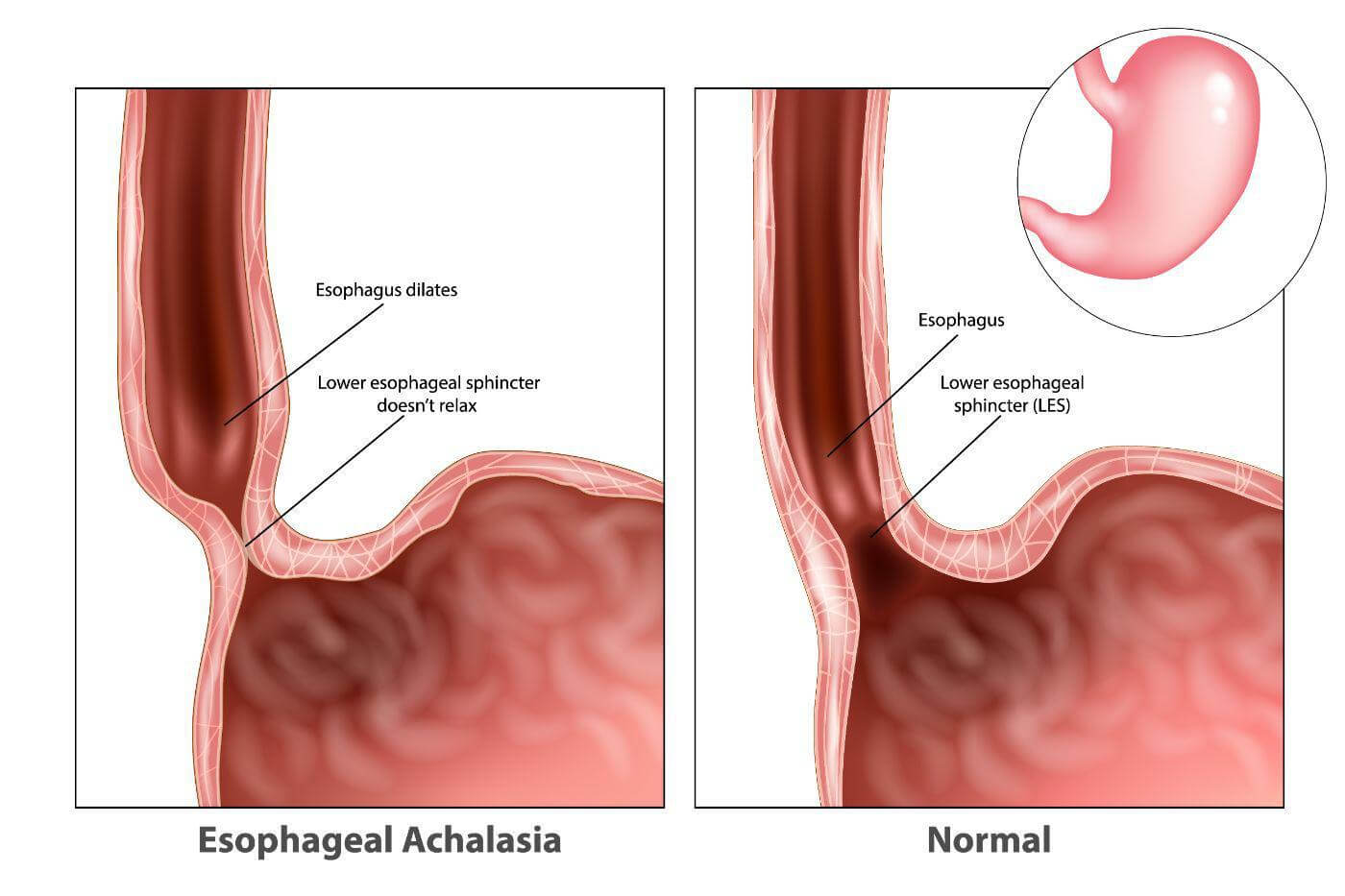 Image source
Image source
Causes of Achalasia
What causes achalasia? Doctors differentiate between two forms of achalasia: primary and pseudoachalasia (secondary achalasia). The occurrence of secondary achalasia is much rarer than that of primary achalasia.
Primary achalasia
Primary achalasia is the most common form. Doctors call it primary achalasia when the cause of the achalasia cannot be clearly identified. How primary achalasia develops is still unclear.
There is evidence that achalasia is caused by the destruction of certain nerve tracts and nerve centers (ganglion cells) in the esophagus. The so-called myenteric plexus (Auerbach plexus) appears to be particularly affected. This is a fine network of nerves in the muscle wall of the esophagus, stomach, and intestines.
According to current research, primary or idiopathic achalasia is probably an autoimmune disease, i.e. a disease with a malfunction of the body’s own immune system.
Pseudoachalasia (secondary achalasia)
Secondary achalasia, however, is caused by cancers of the esophagus or stomach. Most commonly the cause is carcinoma of the gastric cardia.
These diseases damage the nerve tracts in the area of the esophagus so that the normal function of the esophageal contractions and the esophageal sphincter is disturbed.
It is typical of secondary achalasia that swallowing difficulties increase much faster than in primary achalasia. Older people are more likely to be affected by secondary achalasia.
Other conditions that rarely are the cause of pseudoachalasia include metastatic disease, esophageal carcinoma, and an infective disorder like Chagas disease.
How is achalasia caused?
Normally, fluids and food from the esophagus are released into the stomach through a type of valve called the lower esophageal sphincter (LES) by opening and closing muscles.
So after swallowing, it is important that the lower esophageal sphincter open so that the food can pass into the stomach. To do this, the muscles relax at the entrance to the stomach, which is tightly closed regardless of the act of swallowing. This system is controlled by nerves in the gastrointestinal tract.
In achalasia, the lower esophageal sphincter can no longer relax. The muscles remain in a kind of constant tension and prevent the passage of food into the stomach. The esophagus then increases its own pressure from its muscles to push its contents through the tense sphincter.
Since the resistance is too high in the long run, the increased pressure eventually leads to an expansion of the esophagus. The overstretched tissue increasingly loses its functionality and the normal passage of food or liquid is permanently disturbed.
As the disease progresses, the esophagus becomes more and more sluggish and flaccid. In the end, it resembles a functionless sack that is completely immobile.
The dysfunctional esophagus leads to malnutrition and severe weight loss.
Symptoms of Achalasia
Achalasia symptoms typically appear gradually. Initially, the symptoms are usually only mild and occur only sporadically.
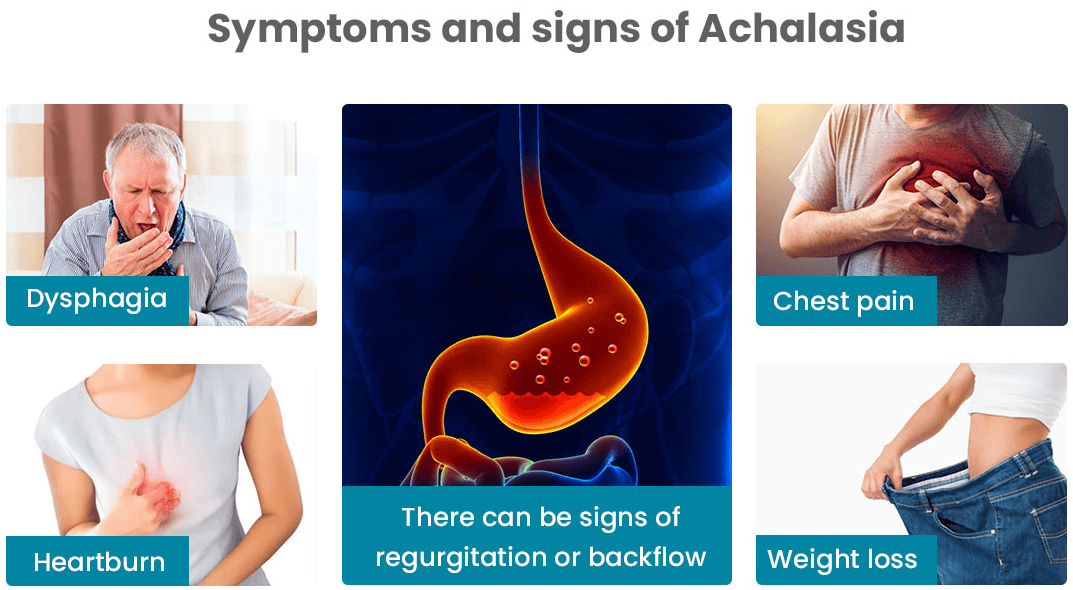
The most common symptoms of achalasia are:
- Dysphagia
The early symptom most commonly experienced.
In the early stages of the disease, patients only experience problems swallowing solid food. While swallowing, they have the feeling that the food is stuck in their throats and accordingly drink more liquids. Increasing the amount of water you drink means the food can get into the stomach a lot easier.
- Chest Pain
In addition, some sufferers experience chest pains that are characterized by a feeling of pressure in the chest region behind the sternum.
The chest pain experienced is similar to heartburn, but treatment generally used for heartburn does not help in this instance.
- Regurgitating of food particles and liquids
Often undigested food remains in the esophagus. When the spontaneous regurgitation of undigested food residues gets into the lungs or throat, it can either result in breathing problems or lead to coughing. Can also lead to bad breath
In an advanced stage of the disease, liquids can no longer be swallowed or only with difficulty. This poses considerable problems for those affected.
Regurgitation gets worse when the affected person lies down.
- Vomiting
Some patients feel very bloated and also vomit.
The patients lack the bitter taste in the mouth typical of reflux disease since the food in achalasia has not yet come into contact with the gastric acid.
Since the lower esophageal sphincter is permanently tense in achalasia, those affected have no or only very rarely heartburn.
- Coughing
Many patients choke on the undigested food when it gets into the windpipe (aspiration).
This happens especially at night when the patients are lying down. The reflux of food can lead to coughing attacks at night. In addition, the food particles in the windpipe and bronchi (aspiration) can cause pneumonia.
- Weight Loss
With pronounced achalasia, those affected lose a lot of weight.
In primary achalasia, body weight decreases slowly over months or years and is usually a maximum of ten percent of the original body weight.
In secondary achalasia, the weight loss can be more pronounced and also progress in a much shorter period of time. Could lead to malnutrition.
Achalasia poses considerable problems for those affected. The swallowing disorder is emotionally very stressful, and when those affected lose a lot of weight, it can significantly reduce their physical abilities.
Who Develops Achalasia?
Achalasia is a rare condition. Those affected include:
- In the US, about one in 100,000 people get achalasia annually.
- Most people who are affected are between the ages of 25 and 60. Can occur at any age though.
- Can develop in children
- All ethnic groups can develop achalasia
- Both male and female sexes are affected equally.
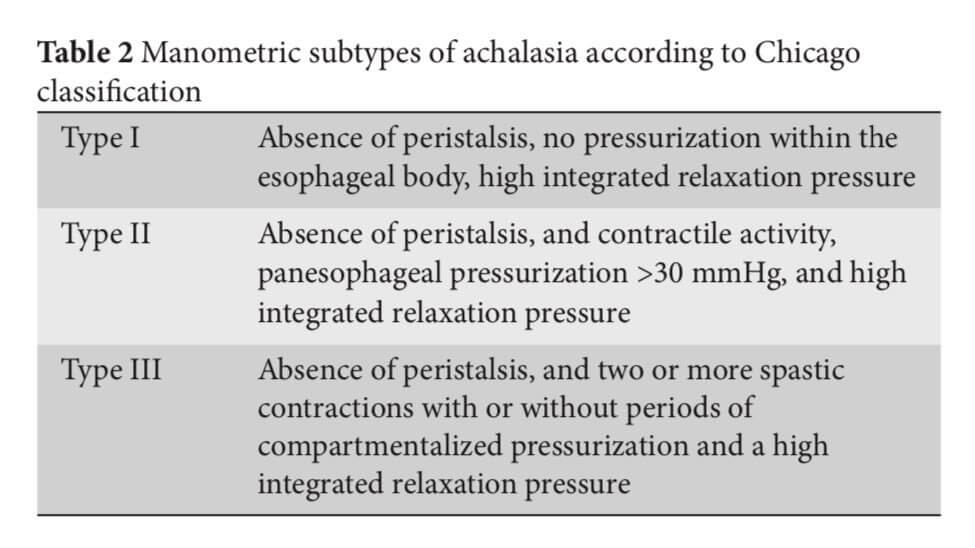
Types of Achalasia
Based on manometric patterns, achalasia is divided into three distinct subtypes, namely:
- Type 1: “classic” achalasia with minimal contractility in the esophageal body. In this instance, the lower esophageal sphincter (LES) does not completely relax causing a little bit of pressure to build up in the esophagus.
- Type 2: intermittent periods of isobaric pan-esophageal pressurization. A more severe subtype of achalasia where food in the esophagus causes pressure to build up, resulting in compression in the esophagus.
- Type 3: presents with premature or spastic distal esophageal contractions. This is the most severe form of achalasia. Symptoms can be so severe that chest pains may be construed as a heart attack. Severe spasms could wake a person from sleep.
Each of these subtypes has its own and different characteristics. Esophageal manometry is used to diagnose each subtype which subsequently helps when the most appropriate treatment needs to be decided upon.
Achalasia Examinations and Diagnosis
If you have had difficulty swallowing, heartburn, or acid regurgitation for a long time, you should see your family doctor.
With a detailed description of your complaints, you provide the doctor with valuable information about your current state of health.
The doctor will examine your abdomen and upper body in particular and shine a light into your mouth and throat in order to be able to determine any changes.
The doctor may also use his/her fingers to detect enlarged lymph nodes in the neck. In order to be able to diagnose achalasia with certainty, further examinations are usually necessary.
If achalasia is suspected, your doctor will refer you to an internist (specialist in internal medicine) or gastroenterologist (specializing in gastrointestinal diseases).
Since the symptoms of achalasia are similar in nature to some other digestive disorders, there are tests that can be performed to assist in correctly diagnosing achalasia.
The 3 tests used are:
- Endoscopy
The structure of the mucous membranes in the esophagus and stomach can be assessed with the help of a reflection through an endoscope.
In addition, the reflection serves to rule out other diseases of the esophagus and stomach such as inflammation, scarring, or cancer.
The patient is not allowed to eat or drink anything for six hours before the examination so that the doctor has a clear view of the mucous membranes during the examination.
Normally the esophagus is then completely empty, but in achalasia, there are often leftovers in the esophagus.
An endoscopy can also reveal small ulcers, yeast infections, and inflammation.
The thin flexible tube of the endoscope, when pushed through the esophagus into the stomach, can be used to check for stomach cancer also.
A tissue sample obtained during the endoscopic examination can be used to check for cancer cells.
Note: “Cancer in the upper part of the stomach can produce symptoms and abnormal manometry results that are virtually identical to those of achalasia. This condition is called pseudoachalasia (meaning “false” achalasia) or secondary achalasia.” Source
- Esophageal swallow test
The esophageal swallow test is a method for displaying the act of swallowing with the help of an X-ray machine and a contrast medium.
The patient swallows a mixture enriched with a contrast agent, usually barium sulfate. While swallowing, the patient’s throat and chest are X-rayed.
If achalasia is present, the x-ray often shows a champagne glass-shaped transition between the esophagus and the stomach entrance.
The entrance to the stomach is thinned in the shape of a pedicel, while the esophagus in front of it is expanded like a funnel.
This champagne glass shape arises because the food pulp builds up in front of the constriction of the lower esophageal sphincter and thus the esophagus in front of the constriction is expanded over time.
- Achalasia manometry
This manometry examination method is the diagnostic tool of choice for achalasia. It measures the pressure in sections of the esophagus brought about by the contraction of the muscles lining the esophagus.
In healthy people, the pressure changes associated with the movements of the esophagus are uniform. Changes in this regular esophageal peristalsis and the insufficient relaxation of the esophageal sphincter can confirm the diagnosis of achalasia.
With the help of a test known as esophageal manometry, the peristaltic movements of the esophagus and the function of the esophageal sphincter can be determined.
In this test, a thin tube is pushed through either the nose or mouth into the esophagus during the swallowing process.
When the lower esophageal sphincter (LES) fails to relax when swallowing takes place and muscle contractions in the esophagus are lacking, achalasia is diagnosed since the esophagus is not functioning properly.
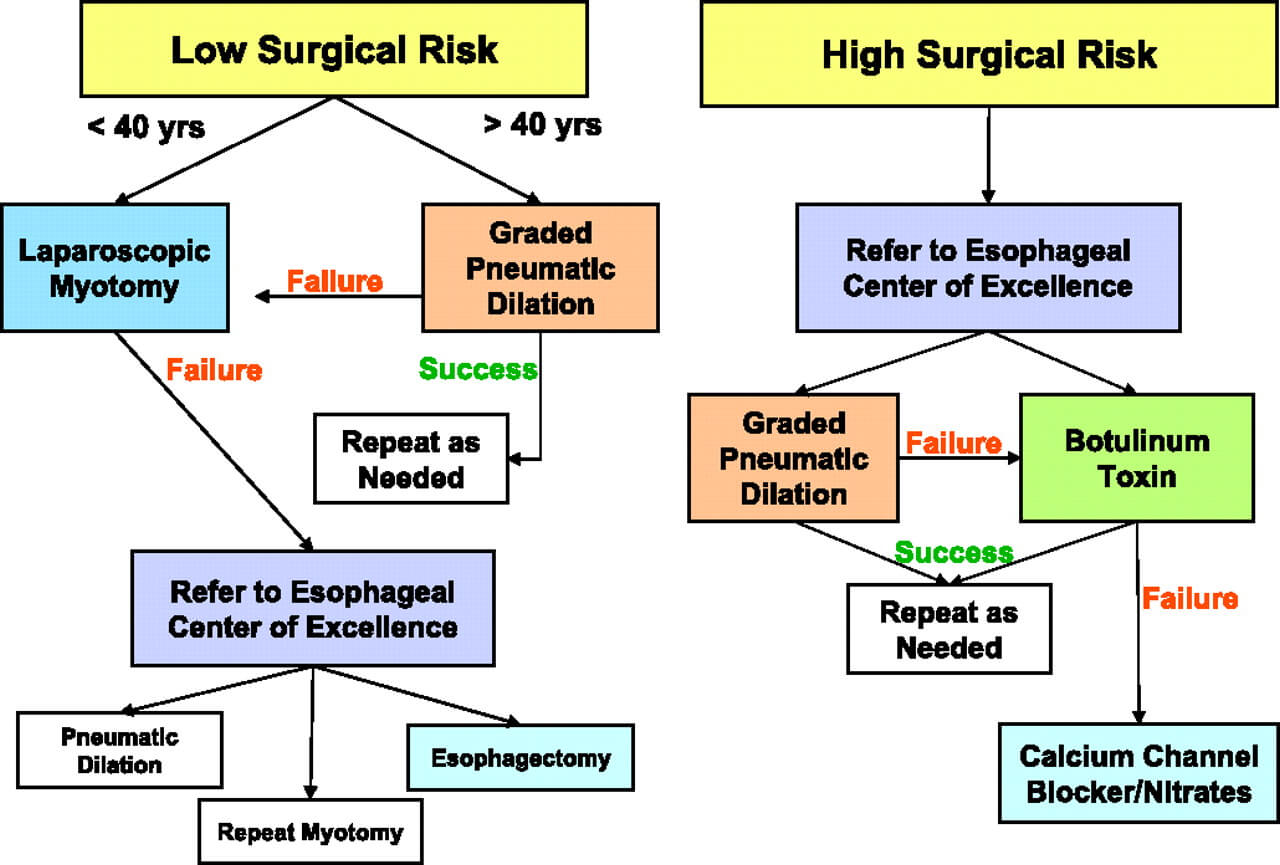
Treatment of Achalasia
There is no cure for achalasia.
The right achalasia treatment can, however, bring relief from the symptoms associated with achalasia.
It is imperative to get treatment. When achalasia is left untreated, the esophagus will eventually stop working; increasing the risk of developing cancer in the esophagus.
Achalasia treatment is necessary if the disorder causes discomfort. There are different options available to alleviate the symptoms of achalasia. With the help of medication or special interventions, an improvement in the symptoms can usually be achieved.
The most suitable achalasia treatment is determined by the severity of the achalasia condition, the patient’s age, and general health condition.
The main aim of therapy is to reduce the increased pressure in the lower esophageal sphincter. Complete healing is hardly possible, however, as nerve cells that have been damaged only regenerate to a limited extent.
Non-surgical Achalasia Treatment:
Pneumatic (balloon) Dilation:
The narrowing of the junction between the esophagus and stomach can be stretched with the help of a balloon. The balloon dilation is performed during an endoscopy, so no surgery is necessary.
Under sedation, the doctor pushes a thin tube through the mouth into the esophagus up to the constriction at the entrance to the stomach. There the small balloon at the end of the tube is inflated. This subsequently helps with the functioning of the sphincter.
Balloon dilation has to be repeated after a few years in about half of the cases.
In rare cases, complications during the procedure can tear the sphincter. Should bacteria penetrate the wound, it can cause esophagitis.
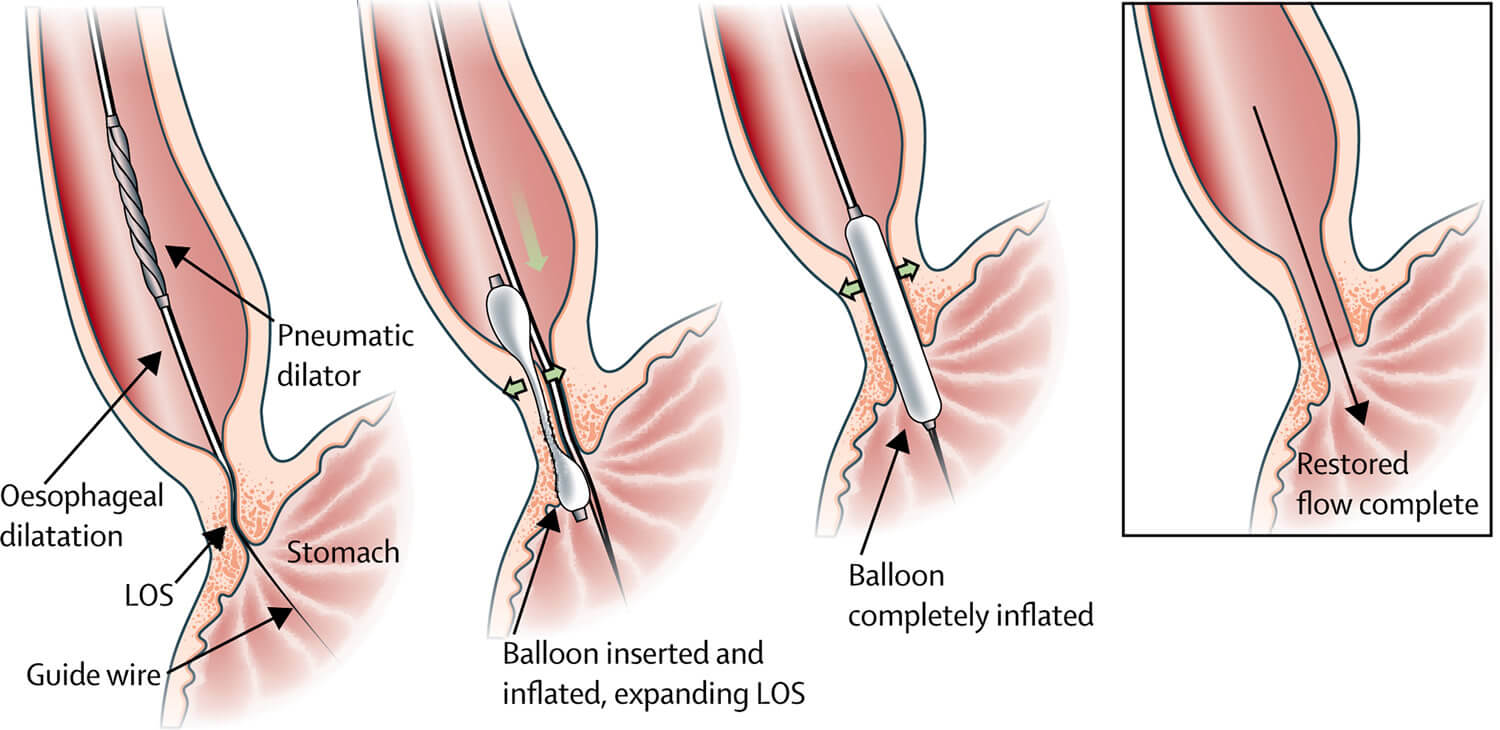
Image source
Botox Injection:
Using an endoscopic needle, the muscle relaxant botulinum toxin type A is injected into the narrowed esophageal sphincter.
Botox injections are, however, best suited for those people who, due to either their age or overall health condition, are not the best candidates for any surgery or balloon dilation treatments.
Most people know Botox as a nerve crippling poison from cosmetic medicine. In the esophageal sphincter, it blocks the nerve tracts, causing the sphincter to relax.
This type of achalasia therapy improves symptoms in 90 percent of those affected. However, achalasia symptoms recur in many patients after just a few months.
When Botox injections are repeated too often, it could have an effect that makes surgery more difficult should the need ever arise.
Medication:
Drug therapy only helps about ten percent of patients.
As a result, it is only used in patients who cannot be treated using balloon dilation or surgery, and where botox injections failed.
The active ingredient nifedipine found in Procardia XL® and Adalat CC® relaxes the spastic esophageal sphincter muscle.
The active ingredient nitroglycerin (Nitrostat) has a similar effect. The medication is taken about 30 minutes before eating. Thus, the lower esophageal sphincter relaxes in time and the food can get into the stomach more easily.
However, with prolonged treatment, the drugs become less effective and further procedures become necessary.
Surgical Achalasia Treatment Options:
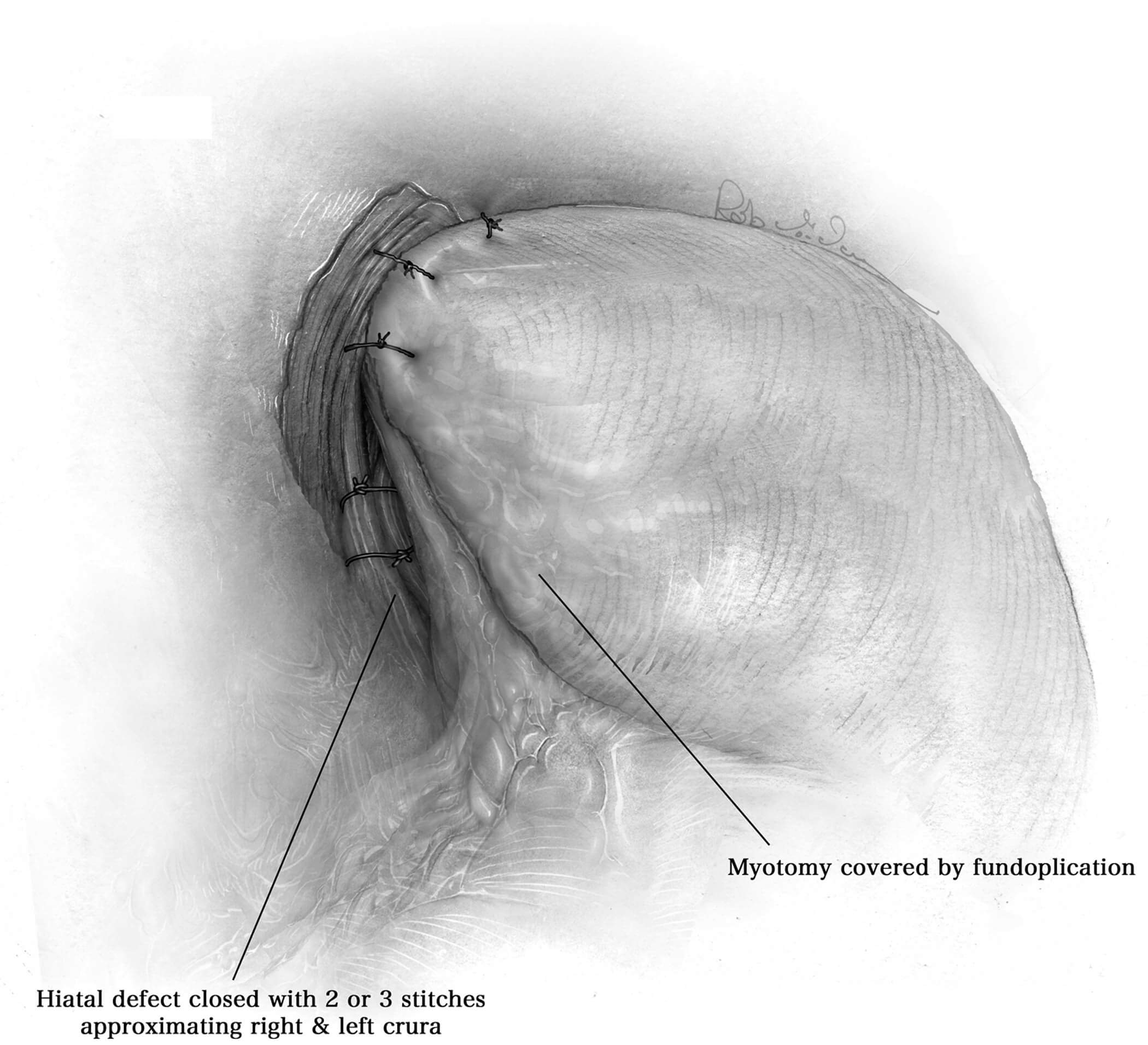
Laparoscopic Heller Myotomy:
The Heller myotomy is a surgical procedure named after the surgeon Ernst Heller. As early as 1913 he performed muscle splitting or myotomy at the junction between the esophagus and stomach. Even today, Heller’s myotomy is the standard procedure for achalasia.
The laparoscopic operation has become routine in achalasia surgery. It is usually combined with another operation, the ventral fundoplication. In fundoplication, an anti-reflux valve is created when the top of the stomach is wrapped around the lower esophagus. On the one hand, this effectively prevents heartburn from occurring after the procedure.
On the other hand, fundoplication has a protective and stabilizing function. The muscle split should be at least six centimeters long on the esophagus and at least two centimeters long in the transition between the esophagus and stomach, in order to achieve good swallowing function.
In up to 90 percent of the cases, the laparoscopic Heller myotomy leads to long-term disappearance or at least a relevant improvement in swallowing difficulties.
Laparoscopic myotomy is a very effective treatment method for achalasia symptoms.
Peroral Endoscopic Myotomy (POEM):
Peroral endoscopic myotomy is a newer surgical procedure, POEM for short.
This is understood to mean incisions in the muscles lining the esophageal wall by means of an endoscope that is inserted through the mouth.
The myotomy is then carried out in this area in the same way as the Heller operation.
Achalasia Prognosis
Achalasia is a chronic disease that unfortunately does not heal spontaneously. The swallowing difficulties typical of achalasia usually increase over the years or even decades. With the help of various treatment options, however, the symptoms can usually be sufficiently alleviated.
Achalasia Complications
If left untreated, achalasia can lead to a steadily widening of the esophagus. In extreme cases, a so-called megaesophagus forms, which is no longer able to transport the chyme from the mouth to the stomach. The increased belching can trigger inflammation of the esophagus (esophagitis) or complications of the lungs (dry cough, hoarseness, and even pneumonia ).
Conclusion
Achalasia is associated with an increased risk of cancer of the esophagus (esophageal cancer).
The risk of achalasia patients developing a malignant tumor of the esophagus is 30 times higher than that of healthy people. This is due to the fact that with constant stress and irritation of the esophageal mucosa, new cells must constantly form to repair the esophageal mucosa.
The increased rate of cell division means an increased risk of cell degeneration. Achalasia patients should therefore be examined regularly even after successful treatment.