
Page Contents
What is acne?
Before exploring the different types of acne pictures let’s first address exactly what acne is…Acne’s most common form is known as acne vulgaris, which means “common acne”, as can be seen in this picture of acne. Acne is generally referred to as pimples, whiteheads, blackheads, zits and blemishes. More severe forms of acne, known as acne cysts and acne nodules, can cause scarring. There is no scientific evidence to support this, but research has shown that millions worldwide are affected by acne. While this condition mainly affects adolescents, many people may be affected by acne well beyond their 30’s, 40’s and even 50’s. Even babies can get acne.
It is a skin condition which occurs when the healthy hair follicles of the pores on the surface of the skin become clogged. Each pore has a hair follicle (small canal) which connects it with an oil gland (sebaceous gland). The glands produce sebum, an oily liquid. The function of the oil is to naturally lubricate and protect the skin by moving dead skin cells to the surface of the skin via the follicles, thus keeping the skin smooth. When too much oil is produced it results in clogged follicular openings (pores). An over production of oil is triggered by various conditions. These include, but are not limited to:
- During puberty, mostly due to elevated levels of the hormone testosterone in both sexes which stimulate the oil glands.
- Lots of sweating and high humidity levels.
- Changes in hormones brought on by stress, pregnancy, menstrual periods, etc
- Drugs can either cause or aggravate acne. These medications include, but are not limited to steroids (Deltazone, Liquid Pred, Prednicen, Orasone), or medications which contain iodides and bromides. Other drugs include Eskalith and Lithobid which are used to treat bipolar disorder. Majority of acne cases are not related to medications however.
- Oil based skin-care and cosmetic products can aggravate the condition. Rather choose a water-based product which won’t clog your pores. Some products have “non-comedogenic” printed on the label; making it easier to find the right product.
- No established evidence exists to link acne and diets high in refined sugars to the development of acne; foods like pizza, fried foods and chocolate are just not advised for maintaining good overall health.
- Some cases indicate that the pressure caused by suspenders, chin straps, collars and helmets can worsen acne.
- Acne also runs in the family. Chances are if your parents suffered from acne, so will you and your siblings.
Many people have found that some of the best acne scar treatments are home remedies which can actually clear up common acne without having to resort to prescription and surgical treatments.
Known symptoms of acne:
Acne generally affects the face, neck, shoulders, back and chest. Many however have been afflicted with acne on their arms, legs and buttocks. Bacteria are not the cause of acne, but when bacteria, dead skin cells and dirt build up, the result is congested pores. Different types of acne appear; the symptoms for each are:
Non-Inflamed Acne:

Whiteheads or blackheads, also known as comedones (koe-muh-DOE-neez). Whiteheads form when pores get totally blocked but generally have life spans of only a few days which means they quite quickly resolve.

Blackheads are the consequence of partially blocked pores and occur when only some of the mixture consisting of oil, bacteria and dead skin cells are allowed to escape through the surface of the skin. The coloration happens when a natural occurring pigment called melanin reacts with oxygen.
“Comedones are forms of acne, which we may more commonly refer to as whiteheads or blackheads. A single whitehead or blackhead is a comedo or comedone, which means glutton in Latin. Comedones is a common plural form of comedo. This type of acne tends to create relatively small black or white bumps on the face. Whiteheads look like they contain a tiny bit of pus, though this is mostly dead skin cells. Although they are still visible, they are called closed comedones because they have a little bit of skin over the top of them. The main difference between a white and a blackhead is that blackheads don’t have this skin closing. This means material in them oxidizes from contact with the air, and turn black or dark brown”. Source: http://www.wisegeek.com/what-is-a-comedone.htm
Papules are tiny, tender bumps and usually concentrated in a single area. The least dangerous type of acne, they can be red, brown, pink or purple. Unless scratched or picked open (which can lead to infection), they are generally painless, and do not hold any pus. Papules should subsequently not be “popped”, as there is nothing that can “pop out”.

Pustules, commonly referred to as pimples or zits, are found under the skin and filled with pus. When properly cared for (keeping it clean by gently washing the area infected with soap and warm water, or using hot compresses which will hopefully open the pores on the surface of the skin sufficiently to allow drainage of the pustule), the pustules pose no threat. You are advised not to pop them; a condition known as acne excoriee (read more here) develops when pimples are popped or blemishes picked. Oftentimes they resolve on their own. When pustules recur, grow larger, or show signs of infection and inflammation, a dermatologist must be consulted. Pustules which get severely inflamed, or are picked at, could cause scarring.
Types of acne pictures:
Inflamed Acne:

Cystic lesions (cysts) is a severe form of common acne (acne vulgaris), and form below the skin’s surface. Cystic acne is the result of clogged hair follicles, which is caused by build-up of excess oil, dead skin cells and bacteria. The acne cysts are large, hard bumps filled with pus as can be seen in the cystic acne pictures. The cysts tend to be quite painful and long-lasting. Popping these will only bring on more pain, and could get inflamed; possibly leading to severe acne scars. Probably the best option in getting rid of cysts is to consult with a dermatologist who will advise on the appropriate cystic acne treatment method to ease the pain and reduce the swelling.

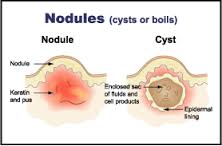
Nodules are similar to cysts, except they have no pus. Known as the most severe form of acne, it is also known as nodular acne. The nodular spots are large, hard and painful bumps that form below the skin’s surface. The pain associated with nodular acne is severe and only dermatological treatment is advised. Do not squeeze the nodules. Behind the nodule inflammation builds up, so does the pressure. The increased pressure now forces the inflammation deeper into the skin. As the inflammation spreads, it causes damage to the skin tissue which disrupts the structure and production of collagen. Loss of collagen and fibrin causes the skin to sink, creating marks on the outer surface of the skin with an ice pick appearance.

Rosacea is a chronic skin condition which is probably more of an embarrassment than it is harmful. That said, treatment is however necessary to prevent the condition from worsening (rhinophyma discussed further down is typically the result of untreated rosacea). Rosacea is associated with both acne vulgaris (in error though: “Rosacea used to be called ‘rosacea acne’ but it is quite different from acne. There are red spots (papules) and sometimes pustules in both conditions, but in rosacea they are dome-shaped rather than pointed and there are no blackheads, whiteheads, deep cysts, or lumps” Source: http://dermnetnz.org/acne/rosacea.html) and seborrhea (dandruff), as well as the eye disorders blepharitis (inflammation of the eyelid) and keratitis (inflammation of the cornea).
People with fair skin and blue eyes between 30-60 years of age are affected. Both sexes are subject to the condition; it is however much more prevalent in women. Initially the redness starts on the face across the forehead, nose or cheeks (as can be seen in the pictures of the condition), but can progress to the ears, scalp, neck and chest. No conclusive evidence as to what causes rosacea exists; some factors thought to contribute include the sun, emotional stress, hot and cold weather, wind, heavy exercise, alcohol consumption, spicy foods, etc.
Typical symptoms of the condition are characterized by the following 4 subtypes:
- Erythematotelangiectatic rosacea is redness of the face brought on by flushing and blushing which can last for 5 minutes. This usually is the first sign of rosacea. Inflammation of the blood vessels just beneath the skin causes the skin to appear red. The skin can also be very dry and flaky. When the vessels become prominent (visible) it is known as telangiectasia “Telangiectasias or angioectasias are small dilated blood vessels near the surface of the skin or mucous membranes, measuring between 0.5 and 1 millimeter in diameter. They can develop anywhere on the body but are commonly seen on the face around the nose, cheeks, and chin” Source: http://en.wikipedia.org/wiki/Telangiectasia)

- Papulopustular rosacea is permanent redness of the face and is the most common sign. The appearance of papules (red bumps) and pustules (swelling with pus) may be mistaken for acne. The skin however is dry and flaky, and no scars form due to these rosacea spots.

Phymatous rosacea is usually associated with rhinophyma which is the enlargement of the nose. Thickening of the skin happens when the sebaceous (oil) glands of the nasal tissue of the tip of the nose become swollen. This thickened skin gives the nose a large bulbous appearance, and generally affects men past middle age. Alcohol consumption is not the cause of the disease, but aggravates the condition.

Ocular rosacea affects the eyes and eyelids. Eyes can be red and dry; eyelids often develop cysts. Eyes are more prone to get infected, and loss of vision and blurry vision may occur. About fifty percent of people, who suffer from the other 3 subtypes described above, also suffer the eye symptoms mentioned here.

Acne Conglobata is a highly inflammatory chronic and severe form of acne vulgaris. Acne conglobata usually affects mostly men between the ages of 18 and 30 years.Found on the neck, face, chest, upper arms and buttocks, they present themselves in groups of 2 or 3 blackheads (comedones). Inflammatory nodules, engorged with a mixture of serum and pus, form around the comedones. The nodules continue to grow and fill with pus; eventually rupturing. After drainage, the lesions fill with pus again. When they rupture, the acne nodules can fuse together and form even larger lesions. Even though scabs form in the centre, they keep on spreading outwards. The lesions remain for a long time, and when they do eventually heal; they leave scars which can be atrophic (the normal type of acne scar) or keloidal (a red, raised formation of fibrous scar tissue caused by excessive tissue repair in response to trauma).

Acne Fulminans, also known as acute febrile ulcerative acne or acne maligna, is a rare and very severe form of acne conglobata. Acne fulminans either develops when acne conglobata is not treated effectively; or the individual already has some form of inflammatory acne. According to the New Zealand Dermatological Society (http://dermnetnz.org/acne/acne-fulminans.html), the prescribed or illegal use of testosterone supplements or the acne medication Accutane (isotretinoin – read more) may also lead to the development of acne fulminans. Acne fulminans typically is the appearance of acne on chest and back of predominantly adolescent males.

The disease primarily is characterized by a sudden development of joint inflammation (arthralgia), fever and ulcerated nodular acne. The inflammation progresses into swollen lymph nodes at the base of the neck. The swelling eventually decreases but goes hand in hand with an increase in the inflammation and swelling of the joints; typically in the knees and hips. Loss of appetite generally sets in, and unless addressed, will cause extreme weight loss and weakening of the muscles.
It is vital to consult with a dermatologist as soon as possible; even the best acne products available over the counter will not cure the condition. Failing to get urgent medical help may cause a serious complication, called SAPHO syndrome, to develop.
“SAPHO syndrome facts
- SAPHO syndrome is a chronic disorder that involves the skin, bone, and joints.
- SAPHO is an acronym for the combination of synovitis, acne,pustulosis, hyperostosis, and osteitis.
- Some researchers feel that the SAPHO syndrome is related to the group of arthritis conditions which typically affect the spine, called the spondyloarthropathies.
- Treatment of SAPHO syndrome typically involves medications which reduce inflammation.
What is SAPHO syndrome?
SAPHO syndrome is a chronic disorder that involves the skin, bone, and joints. SAPHO is an acronym for the combination of synovitis, acne, pustulosis, hyperostosis, and osteitis.
Synovitis means inflammation of the joint lining (synovium). Typically, this is manifests as warmth, tenderness, pain, swelling, and stiffness of involved joints (arthritis).
Acne is a skin condition featuring tiny areas of inflammation with pus formation at the hair follicles. Acne occurs most commonly on the face and upper back.
Pustulosis is a very inflammatory skin condition resulting in large fluid-filled blister-like areas (pustules), typically on the palms of the hands and/or the soles of the feet. The skin of these areas peels and flakes (exfoliates).
Hyperostosis means abnormal excessive growth of bone. The hyperostosis of the SAPHO syndrome frequently is located at the points of the bone where tendons attach, generally in the chest wall.
Osteitis means inflammation of the bone. Patients with SAPHO syndrome can develop inflammation of the sacroiliac joints (sacroiliitis) as well as inflammation of the spine (spondylitis) which leads to stiffness and pain of the neck and back.” Source: http://www.medicinenet.com/sapho_syndrome/article.htm
Gram-Negative Folliculitis, an acne-like skin disorder, (characterized by pustules and cysts), is a bacterial infection. “The term Gram negative refers to the staining pattern of the organisms in the laboratory. Certain bacteria do not take up a stain known as Gram.” Source: http://www.dermnetnz.org/acne/gram-negative-folliculitis.html
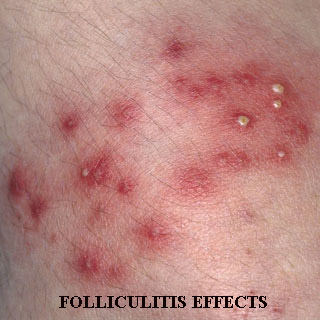
The extended use of certain antibiotics for acne may cause the body to gradually develop immunity against the treatment. This resistance to treatment can bring about a complication in the form of inflammatory acne. When inflammatory acne gets worse, a severe form of acne, gram-negative folliculitis, sets in.
“Why is it Called “Gram-Negative” Folliculitis?
- Gram-negative folliculitis is caused by an antibiotic-resistant bacterial infection, usually after a lengthy, unsuccessful course of intensive antibiotic treatment (usually a topical antibiotic or tetracycline oral antibiotic) for moderate to severe inflammatory acne vulgaris.
- When lab technicians test for bacterial infections, they run the sample through a process called gram staining. Most bacteria will stain blue in the gram test; the bacterial flora normally found on your face is gram-positive, but the particular bacteria that is the culprit for gram-negative folliculitis does not.
- Basically, if you take or use certain antibiotics for too long, this causes what is called bacterial interference. The gram-positive bacterial flora is replaced by gram-negative bacteria that proliferates in your nasal cavities and mucous membranes.
- Klebsiella, Escherichia coli, Pseudomonas, Serratia Marcescens, Enterobacter, and Proteus bacteria are the usual causes of gram-negative folliculitis.
- “Folliculitis” describes the fact that this bacteria inflames the hair follicle.”

The symptoms of gram-negative folliculitis are typically an increase in the severity and number of acne lesions. Cysts and pustules start to develop, especially on the face around the nose, on the chin and cheeks. The skin is red in appearance and looks inflamed. The affected area generally is painful.
Pyoderma Faciale (Rosacea Fulminans) is another rare, but severe form of acne that only affects females between the ages of 20-40 years. What is rather scary about the condition is the fact that it just starts out of the blue, and can affect females who have never even had acne.
The symptoms include unsightly and painful pustules, cysts and red bumps (nodules) which suddenly appear on the chin, cheeks and forehead. Symptoms resemble those associated with both acne and rosacea, but comedones for instance are not present. Those suffering from this affliction may however have acne vulgaris at the same time.

Once started, the condition worsens rapidly, with lesions popping up in a matter of just hours. The lesions are much more severe than those associated with acne vulgaris, in the sense that they tunnel, spread and connect. When these lesions form, they hemorrhage and start to bleed. The crusty scabs that form seep continually, and stick to clothing and linen. The condition may cause fever and aching joints in some individuals; it is however not clear if this is a direct consequence of infection from open lesions or from the condition itself. The condition typically takes about a year to clear up; with scarring almost a given. They are either thick, plaque-like scars, or keloidal.
It is still not known what causes pyoderma faciale.
Acne during pregnancy is quite common. Pregnancy and acne breakouts go hand in hand for more than 50% of women. While anyone can get acne, those more prone to acne breakouts during pregnancy are the ones who have had acne previously and also experience a flare of acne at the start of their menstrual cycle.
Generally speaking acne outbreaks are mild to moderate; some women do however experience severe acne during pregnancy. Acne typically starts in the first trimester; chances are that you will not experience acne during your pregnancy if it does not develop during the first trimester.
As levels of the hormone progesterone, produced by the ovaries, surge, the oil glands produce too much oil (sebum). The follicles, through which the oil and dead skin cells are to be carried to the surface of the skin, become clogged. The dead skin cells and the excess oil now mix with bacteria, resulting in acne.
From the second trimester, progesterone is produced by the placenta. Hormone levels start to normalize, and acne usually starts to clear up. Some individuals may however experience acne throughout their pregnancy.
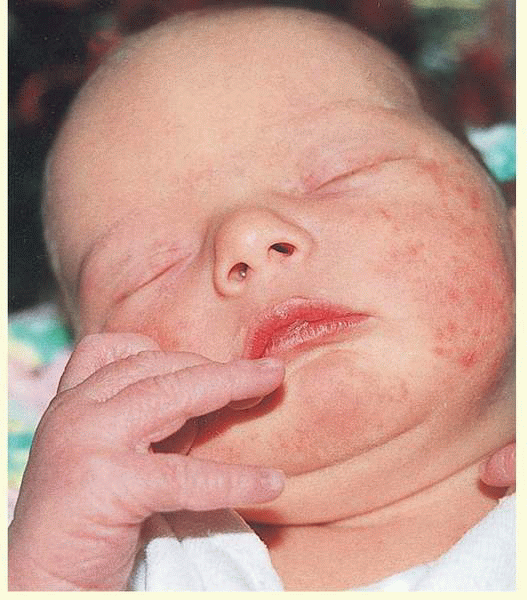
Types of acne pictures: even babies get acne
Baby, newborn baby or neonatal acne is just as common as pregnancy acne, and also harmless. Resembling teenage acne, it generally appears on the cheeks, chin, and forehead, and can last from a few weeks to months. Baby acne is usually characterized by red bumps. The bumps are sometimes surrounded by reddish skin as can be seen from the baby acne pictures below.
What’s causing the acne in infants is not all that clear. Many different reasons are quoted, including:
- Exposure to hormones from the mother while still in the womb
- medications taken by the mother while still nursing
- medications given to the baby
- baby’s clothing washed in too strong detergents
- baby skin-care products
- formula, etc

Acne in infants almost always clear up spontaneously and quickly. When in doubt however, it is always best to consult with your pediatrician. Other skin conditions in newborns that may be mistaken for acne is:
- Eczema “is a chronic itchy skin condition. Eczema usually starts within the first five years of life, most often in the first six months. In babies, saliva from drooling may cause additional irritation, particularly to the cheeks, chin and neck. Treating eczema requires treating both skin dryness and skin inflammation. A good bathing routine is necessary to treat skin dryness. Anti-inflammatory medications, like topical steroids or topical calcineurin inhibitors, are used to treat inflammation. Occasionally, oral anti-inflammatory agents are needed to treat the most severe cases.”
Source: http://www.nationaleczema.org/living-with-eczema/infant-and-toddler-eczema
- Erythema toxicum is a common harmless rash that appears in at least half of all full-term infants. No treatment is needed and it goes away on its own
- heat rash – “Heat rash, also known as “prickly heat” or “summer rash,” is an eruption of little bumps (and sometimes tiny blisters) on the skin that can show up when your baby overheats. The bumps may appear red, especially on light skin. Children of all ages can get heat rash, but it’s most common in babies. If your baby has heat rash, you’ll most likely see it in the folds of his skin and on parts of his body where his clothing fits snugly, including his chest, stomach, neck, crotch, and buttocks. If he wears hats, the rash may spread across his scalp or forehead. How should I treat heat rash? Start by cooling your baby off. Loosen or remove his clothing, and move him into an airy room or a shady spot. You might place him on a cotton towel, which can help absorb his sweat. Apply cool, wet washcloths to the areas affected by the rash. A lukewarm bath with a little baking soda — 2 teaspoons per gallon — can also help. Let him air dry rather than rubbing him with a towel. And don’t use ointments or creams on the rash. These can make the rash worse by trapping moisture. If it’s hot at night, use an air conditioner or a fan in your baby’s room. Direct the fan near your baby but not directly on him. Or place it far enough away so that only a gentle breeze reaches him. You want your baby to be comfortable, not chilled.”
Source: http://www.babycenter.com/0_heat-rash_10881.bc

Menopausal acne, also known as hormonal acne or acne climacterica, develops when the testosterone hormone levels start to rise as the ovaries stop producing estrogen. While hormone replacement therapy’s (hrt) primary function is to restore the imbalance in hormones; it can either cure the acne caused by the imbalance or trigger menopause acne.
Menopausal acne’s appearance is similar to that of acne in puberty. Once again hormones are to blame for the production of excess oil in the sebaceous glands of the hair follicles. Blockage of the pores is caused by the mixture of dead skin cells, excess oil and bacteria in the follicles. The blockage subsequently manifests in blackheads, whiteheads and pimples.
Check out the best products for acne scars..also let us know how the above information helped you. Just like, share or comment below…


